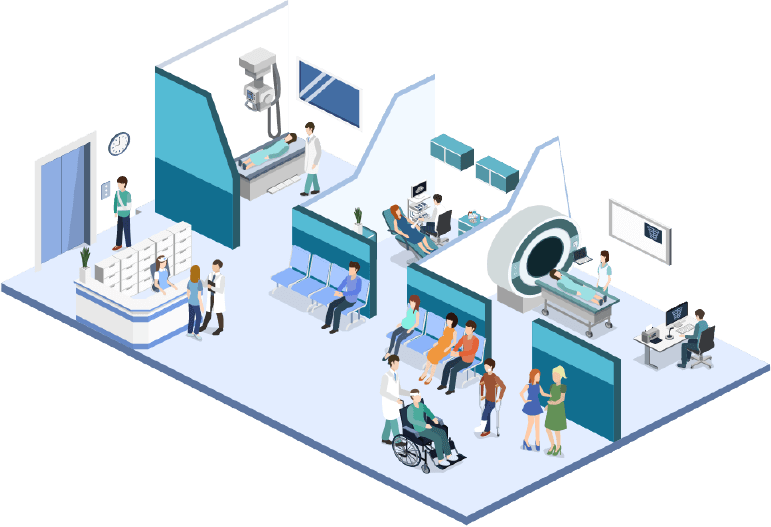
Through our examination of radiology and imaging center patient access workflows, we will provide substantiated improvement solutions that streamline the patient onboarding process from verifying insurance details, prior authorizations, and addressing the recent Clinical Decision Support Mechanism (CDSM) implementation.
By identifying these challenges and outlining the benefits of automated and integrated solutions, using artificial intelligence (AI), and machine learning capabilities where appropriate, we create an onboarding flow that improves the patient’s experience and brings revenue directly to your bottom-line.
Recognizing the current challenges, the Centers for Medicare and Medicaid Services (CMS) extended the mandatory CDSM implementation date to January 1, 2022.1Reporting appropriate use criteria in claims for Medicare Patients. American Medical Association. August 17, 2020.
https://www.ama-assn.org/practice-management/medicare/reporting-appropriate-use-criteria-claims-medicare-patients.
Accessed on August 19, 2020. This extension is intended to give both ordering and furnishing providers ample time to negotiate the technological and workflow challenges before there is a monetary impact.
An Evolving Reimbursement Profile
As the growing trend of consumerism continues to shift the patient care atmosphere, radiology groups around the country are striving to maximize the patient experience through not only their clinical successes but also through their approach to the healthcare payment lifecycle. This balancing act is relatively new and is playing out in radiology groups and hospital systems across the country as the industry shifts to the new reality of patients being more active, and financially responsible, players in their own healthcare.
A major shift in healthcare insurance coverage policy, high deductible health plans (HDHP) are not only here to stay but are increasing in popularity with each successive “open enrollment period” as employees look to reduce their monthly premium costs. HDHPs with annual deductibles of $8K or more per person sound innocuous when people choose the option, but often families don’t have accrued savings able to meet the limits should a member suffer a catastrophic occurrence.
This change is requiring providers to reorient their patient access focus to more fully support the patient. Increasing financial education, estimating amounts due more fully, and reducing surprise billings are some ways that providers are developing these partnerships with patients now and in the future.
Patient Access Defined
For our purposes here, our focus is the initial phase of the healthcare payment lifecycle – patient access – where we examine the steps required to ensure maximum reimbursement as a patient is initialized into a group or department. As the radiology reimbursement landscape evolves and profit margins continue to tighten, forecasting and strategies turn towards new technologies and streamlined procedures as the way forward.
Successful initiatives are focusing on the patient encounter, from the initial patient access point through revenue cycle management (RCM), are renewing interest in the efficiencies gained by automating redundant, time-intensive, manual processes. As an example, industry-wide, over 79% of prior authorizations are still generated and submitted manually22020 CAQH Index – Closing the Gap: The Industry Continues to Improve, But Opportunities for Automation Remain. Published by CAQH Explorations, 2021. Retrieved 2/2/21 from
https://www.caqh.org/sites/default/files/explorations/index/2020-caqh-index.pdf even though insurers have the capability to process them electronically.
Defining Access Components by Function
Insurance Verification & Benefits
It is critical that accurate and current patient demographic3Berg, S., May 15, 2018. Improve health equity by collecting patient demographic data. Retrieved from the American Medical Association on 1/9/2020 at
https://www.ama-assn.org/delivering-care/population-care/improve-health-equity-collecting-patient-demographic-data and insurance information is collected and used to onboard the patient into the reimbursement system to ensure valid billing information is obtained regarding:
- Insurance eligibility dates
- Co-pays and co-insurances
- Deductibles
- Secondary insurance and coordination of benefits
- In-network vs. out-of-network coverage
- Referral requirements
- Prior authorization requirements
Without this key information, revenue reimbursement may be denied through the contracted insurance payers.
Patient Pay Estimates
Today, fully 35% or more of the cost of healthcare may be the patient’s responsibility – service you provide and should be compensated for – and the patient should be aware of this amount before entering your practice. While there are always unforeseen circumstances that arise, a large percentage of costs can be well researched and pinpointed ahead of the actual visit.
It has long been customary for many practices to notify patients of pending amounts due as they arrive, which is often a shock to the individual and sets up an adversarial relationship from the start. But what if you are proactive in notifying your patients about payments ahead of an appointment and requesting payment at that time, thereby allowing them time to arrange or budget as needed?
This allows the patient to digest the amount, ask questions, research their insurance plan, and become an active participant in the process. It also encourages your staff to identify potential concerns and to offer arrangements that reinforce an obligation, such as 50% now-50% at the time of service or third-party financial plans.
Clinical Decision Support Mechanisms
Appropriate Use Criteria (AUC) and CDSM has entered the education and operation testing period lasting until the end of 2021. This will require changes to the diagnostic process (to include consulting AUC) and billing procedures (certificates of adherence) for advanced imaging tests ordered for Medicare-eligible patients. While inpatients and certain emergency patients are excluded from this change, all other Medicare patients fall into the CDSM category, whether in a hospital setting, group practice setting, or imaging center.
The unique structure of the CMS-defined process presents challenges for the providers performing the tests since they are financially responsible to code claims based on having received the CDSM certificates from their ordering provider. However, they are relying on the ordering provider to consult the AUC and then generate and forward the actual certificates themselves via their software through CMS-approved vendors4Centers for Medicare & Medicaid Services (CMS), January 2020. Appropriate Use Criteria Program – Clinical Decision Support Mechanisms. Retrieved from CMS.gov on1/9/2020 at
https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Appropriate-Use-Criteria-Program/CDSM.
Prior Authorizations
The prior authorization process is probably the least appreciated function that takes place in any practice. It is rightfully seen as disruptive to the patient’s care and experience, a roadblock to necessary procedures and equipment (often determined after the patient encounter), and an uncompensated use of physician and staff time5American Medical Association, 2019. Prior Authorization Practice Resources. Retrieved from the AMA on 1/5/2020 at
https://www.ama-assn.org/practice-management/sustainability/prior-authorization-practice-resources.
A recent AMA Prior Authorization Physician Survey6American Medical Association, 2019. Prior Authorization Practice Resources. Retrieved from the AMA on 1/5/2020 at
https://www.ama-assn.org/practice-management/sustainability/prior-authorization-practice-resources found that 92% of patients experience a care delay due to requirements for preauthorizations. And equally troubling, that a significant number of patients abandon care altogether, negatively affecting clinical outcomes.
As previously stated, further complicating the prior authorization process is the fact that according to the “2020 CAQH Index on Closing the Gap: The Industry Continues to Improve, but Opportunities for Automation Remain”, only 21% of providers are using a fully automated electronic process7Ibid, 2.. This means that an average of 15 hours per provider of staff time per week is used to process the required prior authorizations8American Medical Association, 2019. Prior Authorization Practice Resources. Retrieved from the AMA on 1/5/2020 at
https://www.ama-assn.org/practice-management/sustainability/prior-authorization-practice-resources manually.
How to Maximize Revenue by Leveraging Automation
With what’s available today, it’s important to define the three types of technology and outline how each could benefit the process of patient access flow. Using HL7 or API-based integration that guarantees 100% HIPAA compliance, functions are completed in real-time, followed up as necessary, and status automatically reported at completion.
Automation – eases the redundant human burdens and mimics the actions of the workforce. Automation is being used to determine insurance verification and benefits, prior authorizations, and patient responsibility for pre-collections.
Analytics – digital data collection designed to enhance productivity through analyzing patterns, trends, and statistical information. Data analytics is being used to quantify outcomes based on performance and developing predictive scenarios to enhance RCM results.
Artificial Intelligence – by identifying patterns through computational analyses, AI can make predictions that support and amplify those made by humans alone. For patient access, this means predicting risk and behavior and forecasting potential outcomes for RCM purposes.
Best Automated Practices for Patient Access
The efficiencies recognized and benefits enjoyed by automating each function within patient access during the onboarding process include increasing revenue captured, savings or redirection of front and back-office professionals’ time, reduction in denied claims and follow-up, and a vast improvement to the patient experience.
Insurance Verification and Benefits
Automated insurance verification solutions are among the most valuable technologies that a radiology group or imaging center can implement to enhance their patient access workflow. Accurate and immediate verification of a patient’s eligibility is paramount in kicking off the entire reimbursement process. With automated eligibility and remaining benefits verification, your admissions professionals can proceed with efficient scheduling meeting the patient’s needs quickly.
As the basis for any efficient RCM system, the patient insurance information should be gathered thoroughly with copies of insurance cards and ID’s becoming part of the patient’s permanent records and double-checked at each visit. Today’s automated processes allow the insurance to be verified before the patient’s visit and, again, when the patient arrives to ensure that no changes in eligibility have occurred and an up-to-date remaining deductible amount is obtained.
Additionally, insurance verification and eligibility through an automated software solution not only greatly reduces the administrative burden of manual verifications, but also can be integrated with prior authorization and patient pay functions. A verification solution will reduce denials rate, significantly cut down on A/R days, allowing staff to be reallocated to more patient-centric positions.
But there is also another equally important process that takes place during this initial scheduling phase – educating the patient on the practice’s financial policies, including payment expectations, cancellation policies, collections procedures, and missed appointment charges. You will have other opportunities to reinforce your practice guidelines, but it’s important to convey the information upfront.
Patient Pay Estimates
Once your admissions professionals have secured a valid PA and verified eligibility, an automated patient portion estimate now becomes available, and patients can be informed of their financial obligation. At this point, the onboarding staff can proceed to collect the amount estimated to be due according to your well-defined financial policies, i.e., collection, payment plans, financing, etc.
Clinical Decision Support Mechanism
Looking through the practice lens of radiology, the AUC program and CDSM were conceived as a process that would complement and elevate the referring provider’s diagnostic practice, strengthen the Medicare patient experience, and reduce needless advanced image testing. The requirement impacts all physicians, APP, and facilities that are billing Part B Services to Medicare9CMS, July 1, 2018. Appropriate Use Criteria for Advanced Diagnostic Imaging – Voluntary Participation and Reporting Period – Claims Processing Requirements – HCPCS Modifier QQ. Retrieved at CMS.gov on 7/12/2019 at
https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM10481.pdf. Note that exclusions are being made for emergency patient encounters, inpatient services billed through Part A, and ordering professionals with significant hardship, such as rural proximity to services.
When reviewing and evaluating a comprehensive CDSM package from the CMS published list of approved vendors, consider a partner that offers these valuable components:
- A comprehensive and up-to-date library of AUC’s sourced from multiple qualified Provider Lead Entities (qPLE’s)
- A bi-directional, integrated clinical dashboard that provides immediate access to current patient information for both
furnishing and ordering physicians - Coverage of all priority clinical areas as detailed by the CMS, including coronary artery disease (suspected or diagnosed),
suspected pulmonary embolism, headache, hip pain, low back pain, shoulder pain (to include suspected rotator cuff injury), cancer of the lung (primary or metastatic, suspected or diagnosed) - Ability to support referring providers within their EHR/EMR systems
- Ability to generate compliance certificates required for reimbursement
- A qPLE that meets all security requirements and HIPAA compliance standards
CMS has extended the mandatory CDSM implementation date to January 1, 202210Ibid 1.. This extension is intended to give both ordering and furnishing providers ample time to negotiate the technological and workflow challenges before the full monetary impact.
Prior Authorizations
With intuitive and seamless processing of prior authorizations in real-time with full transparency, automation and AI-driven technology allows requests to be submitted to the appropriate payer, monitored and followed up, and alerts and notifications updated continuously. By automating the prior authorization process, significant time is saved by eliminating manual, burdensome workflow.
To proactively address the multi-layer issues surrounding preauthorization, it’s helpful to identify the challenges you’re currently experiencing in the overall prior authorization process. Once those have been isolated, then rethinking your workflows and zeroing in on a solution becomes more effective.
With a deliberate and strategic approach, you can improve patient access and see benefits in the healthcare billing lifecycle workflow, including:
- Prior authorizations processed in real-time
- Scheduling the patient at the time of service
- Lower denial rates
- Increased revenue
- Improvements to A/R and days outstanding
Obtaining a prior authorization continues to be an ongoing struggle for most radiology groups today. The process is labor-intensive and time-consuming, often requiring many hours of constant follow-up by your staff that takes time away from patient care. With improvements in today’s technologies, new software options are being implemented in radiology groups around the country that are capable of processing prior authorizations in real-time, eliminating inefficiencies in obtaining care and capturing revenue that has been previously forfeited.
A Case Study in Radiology
A highly successful outpatient radiology group with a large medical imaging center specializing in full major modality scans, specifically CT, PET, MRI, and Nuclear Medicine, was experiencing an overwhelming volume of prior authorization demands from referring providers (>70%). Once they implemented a scalable solution offering total automation of the prior authorization workflow, an intuitive interface with cloud-based access, and expedited support for emergent requests they recognized the following improvements:
- Faster turnaround time for prior authorizations and expedited scheduling
- Increased revenue by $750-$1,000 per day
- Reduced patient migration with more competitive prior authorizations by 30% per day
- Significantly reduced manual tasks and administrative time
- Strengthened relations with referring providers and practices
Summary and Conclusion
While many in radiology feel they already have effective and extensive experience in onboarding patients, today’s technology offers improved and streamlined opportunities to assimilate patients efficiently. These automated solutions not only improve the patient’s experience during pre-registration but significantly impact RCM in a positive and worthwhile way to the end result—an improved bottom line.
Best-in-class systems using automation, artificial intelligence, and machine learning using a predictive rules algorithm based on payer guidelines, which determines the next best action as well as implementing a reimbursement strategy, will yield maximum revenue capture. This allows providers and staff to commit to higher-level functions that genuinely improves the patient care continuum.
Today, a healthy and robust radiology group relies on state-of-the-art operational workflows to ensure maximum revenue reimbursement. These patient access solutions along with industry best practices, make for an efficient front-end revenue cycle.
To learn more about best practice patient access solutions and how it can transform your healthcare revenue lifecycle workflow, contact us today.
Thanks for reading. If you’d like to see the footnotes, please download this white paper as a pdf here.
From insurance verifications to prior authorizations, patient access sets the tone for reimbursement. Is your radiology group meeting (and exceeding) your financial goals?
Download a PDF version of “Guide to Automated Patient Access for Radiology” to reference later and read more below.
