Addressing the Hospital Prior Authorization Burden

With the insurance industry unrelenting on reducing or streamlining the prior authorization process, hospitals and healthcare systems continue to struggle with the operational implications of a burdensome and redundant system. It’s time to consider an advanced automation solution that offers real-time processing integrated with the EHR/EMR and billing system. Using artificial intelligence and machine learning capabilities, digital prior authorizations improve patients’ access to care, and relieve clinician frustrations.
Can Prior Authorizations Be Brought Under Control?
It doesn’t matter if your providers have recently completed their training or have been board-certified providers for many years; prior authorizations are a necessary step that simply can’t be avoided. While the symptoms requiring therapeutic intervention are undeniable, insurance companies will require providers to document the necessity of treatment before agreeing to reimburse.
Prior authorizations create frustration in a variety of ways, including:
• Delaying patient care for up to three or more weeks
• Causing a provider to alter their treatment plan for expediency
• Being more susceptible to review and rejection because of insurance company bias
• Being administratively burdensome, taking several hours to several weeks to complete
• Negatively impacting the scheduling process and, ultimately, the patient experience
Recent Calls for Change
The American Hospital Association (AHA) recently called on the Centers for Medicare and Medicaid Services (CMS) to improve prior authorizations, stating that they strongly recommended changes that would reduce administrative burdens placed on their membership in their efforts to increase advocacy efforts.
Additionally, the AHA signed onto the American Medical Association (AMA) letter1Letter to the Honorable Seema Verma, Administrator, Centers for Medicare & Medicaid Services, US Department of Health and Human Services. September 20, 2019.
https://j2vjt3dnbra3ps7ll1clb4q2-wpengine.netdna-ssl.com/wp-content/uploads/2019/10/AMA-Prior-Authorization.pdf. Accessed on July 29, 2020. expressing strong concerns to the House of Representatives Committee reviewing H.R. 3107, the Improving Seniors’ Timely Access to Care Act2DelBene, S. H.R. 3107 – Improving Seniors’ Timely Access to Care Act of 2019, 116th Congress (2019-2020). House – Ways and Means; Energy and Commerce Committees, Congress.gov. Introduced in the House on June 5, 2019.
https://www.congress.gov/bill/116th-congress/house-bill/3107. Accessed on July 3, 2020., meant to streamline and standardize the prior authorization process through Medicare.
While the American Healthcare Insurance Plans (AHIP) group has signed on to support all of the initiatives, insurance payers have been clear that prior authorizations are seen as an effective tool that helps contain costs, and manage the care being delivered and the industry has seen the use of prior authorizations increase, not decrease. According to the Medical Group Management Association (MGMA) 90% of healthcare leaders report that payer prior authorization requirements are increasing with no end in sight3Ernst, C., JD. Prior authorization pains growing for 9/10 physician practices. Medical Group Management Association, MGMA Stat, Federal Compliance. September 19, 2019.
https://www.mgma.com/data/data-stories/prior-authorization-pains-growing-for-9-10-physici. Accessed on July 12, 2020..
While there has been growing discord about prior authorizations for several years with major governmental and industry representative bodies joining the chorus, little has changed. Even if foundational improvements are considered, the prior authorization process will likely continue in a new form, but still, require clinician and administrative time to manage. Being proactive in facilitating an efficient process seems to be the best solution.
Manual Processes Slows Down an Already Cumbersome System
The time involved in processing prior authorizations siphons valuable resources away from where it’s needed while business staff process redundant paperwork, sit on hold while waiting for turns, and faxing paperwork all in the hopes of obtaining a quick answer. As documented in the 2019 CAQH Index4Ernst, C., JD. Prior authorization pains growing for 9/10 physician practices. Medical Group Management Association, MGMA Stat, Federal Compliance. September 19, 2019.
https://www.mgma.com/data/data-stories/prior-authorization-pains-growing-for-9-10-physici. Accessed on July 12, 2020., over 87% of healthcare providers use a manual system that is overly burdensome.
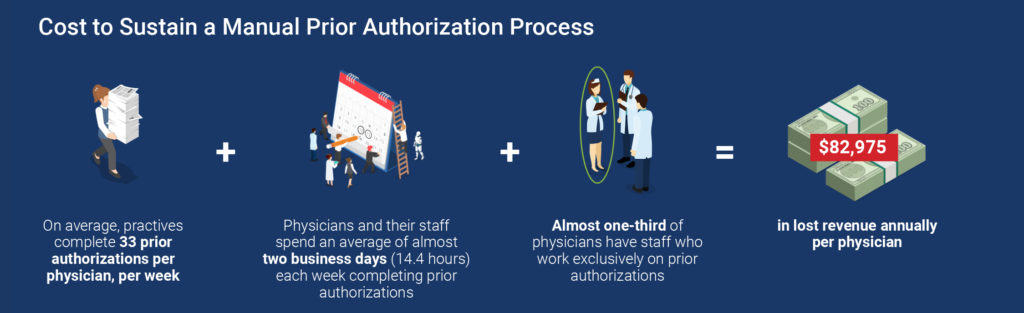
Today, prior authorizations are required for many procedures, tests, and medications throughout healthcare — and hospitals and healthcare systems are no different. Many treatment options all need prior authorizations before the provider can begin to treat the patient. By handling the needed prior authorizations manually, it’s estimated that, on average, over two full days of administrative time per provider are required.
of medical practices use a manual system to manage prior authorizations
3 Ideas to Make the Prior Authorization Process More Effective
Regardless of the industry stakeholder intention, it doesn ’t appear that prior authorizations will go away completely. Rather it’s more likely that insurance companies will reign supreme, and they will continue in some (hopefully) streamlined form.
No matter how frustrating, prior authorizations do seem to help curb healthcare costs. So the question may be how to make them effective in a hospital or healthcare system setting while reducing the administrative burden/costs and improving revenue? Here are three ways to make the process more functional:
1. Always submit organized, clear documentation
Understanding that insurance will likely question many requests for services, documentation becomes key, including all provider clinical notes.
Implement a protocol or EHR/EMR template that ensures comprehensive documentation. Understand and stay ahead of what they are going to request, making sure to fully complete prior authorizations.
2. Be prepared for clinical review
Most insurance payers will elongate the approval process calling for clinical review or outright reject the request. On the other hand, most insurance payers don’t even require a prior authorization on certain less intensive treatment options signaling their strong desire to funnel patients to that alternative regardless of appropriateness.
Be ready to submit organized, concise, well-articulated appeals with all supporting information. Under the Affordable Care Act, all insurance payers are required to have an appeal process in place. Ask for a 72-hour expedited or urgent review to speed the process along even further.
3. Consider a fully-automated prior authorization process
Engaging advanced automation means using AI-driven software that is secure, comprehensive, and fully electronic. Linked to the EHR/EMR system, prior authorization information can be collected, submitted, and followed up 24/7, in real-time.
When using a fully automated prior authorization system, there is a significant opportunity to reduce administrative time and costs, and schedule patients much more efficiently. Should an appeal be needed, an automated system would generate and submit the appeal based on pre-defined parameters with associated documentation.
Improving the Prior Authorizations Process for Hospitals and Healthcare Systems
Using up-to-the-minute advanced automation, Prior Authorization Software, that uses ar tificial intelligence and machine learning capabilities, is the most beneficial solution.
To outline, cloud-based, AI-driven software can be integrated bi-directionally with the hospital’s EHR/EMR and billing system. As soon as the patient’s order is input, evaluations, and treatment requiring prior authorizations would be electronically identified, provider/facility detail, patient demographics, and test/diagnosis information would be collected, and an approval request submitted to the insurance payer portal required.
AI-driven software with machine learning capabilities would acce ss continually updated insurance information clearinghouses storing thousands of insurance groups and plans. Each with their own unique guidelines and requirements and electronically determines the prior authorization parameters for routing the request. Prior authorization approvals that once took between a couple of hours t o several days or weeks can now be accomplished in seconds with a 98+% accuracy rate, as documented by an Infinx case study.
Let’s take a focused look at the impact aut omated prior authorizations can have in hospitals:
- Initial Processing — From the moment patient information is entered into the EHR/EMR system; guided processes monitor key identifiers to initiate the prior authorization. Matching ordered tests or medications while constantly updating insurance prior authorization requirements, the system stands ready to gather the required information and submit the request in real-time.Business or clinical staff no longer need to manually process forms, wait on hold, or fax repeatedly, and can refocus their time on higher-level functions.
- Continual Follow-Up — Once the prior authorization approval has been submitted, electronic follow-up occurs 24/7 until a final resolution is obtained. If additional information is required or an appeal is necessary, the practice is notified immediately so that a response can be crafted and submitted as soon as possible.
- Dashboard Notifications — Waiting for insurance payer responses has historically been a time-consuming affair that took hours of manual follow-up and burdensome administrative effort.
With an interactive dashboard, today’s AI-driven Prior Authorization Software gives a practice snapshot clarity on all active prior authorization requests so that patient and clinician questions can be answered, and follow-up made immediately.
- Scheduling — Alleviating the frustrations of having to schedule and reschedule patients based on prior authorizations, a hospital or healthcare system would have much more accurate parameters to allow a more efficient process for everyone improving the patient’s experience and allowing the providers to focus on providing care.
- AR and Claims Management — With less prior authorization problems comes less rejected or denied claims, possibly up to 31% fewer according to MGMA, and more revenue is hitting the bottom line5Ibid. iv.. As a bonus, AI-driven software exists to handle denied claims like prior authorization solutions with a >95% quality standard according to Infinx.
- Analytics and Reporting — Bringing full transparency to future operations, timely analytics, and reporting pinpoint any breakdowns inefficiency or areas needing improvement so that future patients benefit from an even better experience.
The Overall Cost Savings Available
According to the 2019 CAQH Index, each individual prior authorization industry-wide costs, on average, $14.24 to facilitate manually, while using an electronically automated system would cost $1.93 per PA6Ibid. v.. This is a savings of $12.31 per prior authorization and untold hours of frustration and rework.
The trickle-down effect would be a reduction in denied or reject claims that are currently left unresolved or abandoned with overwhelmed business staff lacking the time or understanding to pursue.
Is This Type of Electronic System Secure?
Using the Infinx Prior Authorization Software platform, a seamless and scalable solution is created that uses Health Level 7 (HL7) or Application Program Interface (API) based integration and is compatible with all leading EHR/EMR, and hospital billing systems. The Infinx Prior Authorization Software solution embeds all Patient Health Information (PHI) in layers of security that is Electronic Data Interchange (EDI) compliant and stores the data on the cloud using 64-bit and 256-bit encryption that guarantees 100% HIPAA compliance7,Napco’s iBridge Technology Named Top Innovation of 2014 by Security Sales & Integration Magazine – Recurring Revenue Model Makes iBridge a Top Choice for Security Dealers. January 13, 2015.
https://investor.napcosecurity.com/2015-01-13-NAPCOs-iBridge-Technology-Named-Top-Innovation-of-2014-by-Security-Sales-Integration-Magazine. Accessed on February 3, 2020.8Integrating Prior Authorization Solution with Epic PMS While Protecting PHI at a Pennsylvania Hospital Group. Infinx Case Study. 2018. https://oldinfiwebsstg.wpengine.com/resource-casestudy/integrating-preauthorization-solution-with-epic-pms-lt/. Accessed on February 2, 2020..

In Summary
As prior authorizations continue to grow, differentiating your hospital or healthcare system from others by offering pristine business support to referring providers or self-referral patients helps in securing future potential patient growth. Your referring provider base will see the benefit to their patients with more timely care initiation and less cumbersome reimbursement.
While healthcare associations and government entities continue to discuss streamlining prior authorizations, it seems clear that the process itself will remain in place as a way for insurance payers to control care. Meeting the challenge seems a more prudent and proactive response instead of waiting for change to occur.
Is your hospital or healthcare system struggling with the operational consequences of inefficiency prior authorizations? It’s time to consider an advanced automation solution that improves patients’ access to care and relieves providers’ frustration.
Download a PDF version of “Addressing the Hospital Prior Authorization Burden” to read later or scroll down and continue below.