There’s a lot of buzz and hype today around artificial intelligence (AI), and it has definitely become a mainstream term in the healthcare industry. It’s been estimated that AI is roughly an $8 billion market today, and is expected to exceed $106 billion within a few years, so it’s no surprise that the healthcare industry is making AI a priority.
In a 2017 study conducted by the American Medical Association, 84% of survey participants described the burden of prior authorization on physicians and staff as high or extremely high. Other studies have suggested that physicians spend an average of 20 hours per week and nearly $83K per year interacting with insurance plans, and fixing prior authorization issues. With the prevalence of prior authorization requirements on the rise, these numbers will continue to climb.
This blog will review the benefits of automation, and how AI can help with overall workflow improvements by allowing your staff to focus on billable patient care versus costly administrative tasks. Imagine the efficiencies that could be achieved if your workflow of manual prior authorizations could be automated.
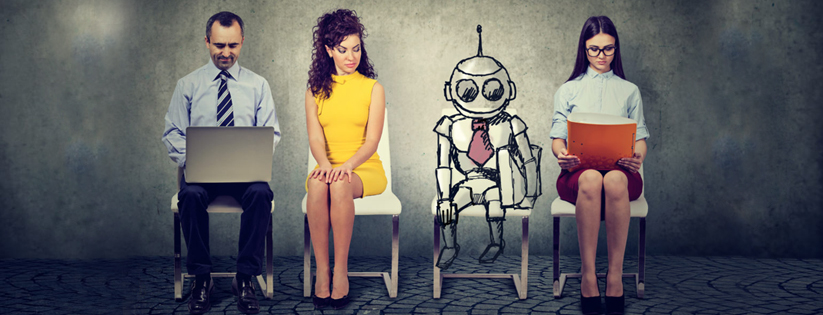
Man and Machine Will Transform Your Revenue Cycle
The revenue cycle is the backbone of any healthcare organization and contains a variety of manual patient access workflows and processes, which are opportune tasks for AI and automation. For example, checking a patient’s insurance eligibility, deductibles, and prior authorization requirements. The ability to automate tasks that once took significant human resources changes the game for hospitals, clinics, and medical imaging centers.
AI can be defined as the mere ability to mimic human behavior with the primary goal focused on developing systems to help people make better, faster decisions and actions, while continuously learning. AI is great at processing data, but bad at thinking in abstract. In reverse humans aren’t so great at processing large amounts of data or storing information; but great at abstract thinking. When automation and AI reaches its limit, you need a human to step in and complete the process. AI will help us streamline, speed up, and basically give us error-free workflow solutions; however, we still need the help of humans to determine the context of the data provided.
AI and human intelligence (HI) complement each other, together they perform tasks that machines can’t do alone by reducing manual processes and risks, and increasing consistency and productivity. You need machines to analyze and crunch the data and build patterns, automation to optimize your workflow, and the expertise of humans to manage complexity and to make better, informed decisions together, ultimately improving and transforming productivity in healthcare.
Why It’s Important to Streamline Your Prior Authorization Process
It’s an understatement to say that the healthcare revenue cycle management is a complex function, because it is in fact the most important function for the fiscal health and well-being of any healthcare organization. The only way to survive onerous prior authorization burdens is to optimize accuracy and maximize revenue through electronic, automated prior authorizations. Best practices in prior authorization are built on software that delivers the following benefits:
- Timely prior authorizations conducted at the time of patient scheduling
- Accurate prior authorization details obtained for accurate claim submissions
- Automated prior authorization tasks, reducing physician admin time
- Cloud-based tools that provide real-time data to make good decisions about patient payment and scheduling
There are many benefits for AI and automation in a healthcare revenue cycle due to its ability to execute repetitive, high-volume tasks that are prone to human error. When you optimize the amount of information you have and maximize its timeliness, the results are more accurate claims and fewer denials, which equates to more revenue for your practice.
Intelligent Automation
The best solution for streamlining your prior authorization process is when your workflow is automated for real-time decision making.
There are a number of considerations for healthcare organizations to think about when implementing an AI solution for their revenue cycle management. Infinx is leading the way with AI with the Infinx Patient Access Software solution, which reduces payment defaults, denials on preauthorizations and claims, and improves schedule optimization. It can dramatically improve the accuracy and speed of your patient access workflow. The Infinx Patient Access Software solution includes a preauthorization module, with seamless HL7 integration with your EHR, and a vast network of clearinghouse integrations. The solution is cloud-based, using AI to optimize your prior authorization process, and HI to manage the complexity of exceptions.
Prior authorizations are not likely to go away anytime soon, so by automating the process, prior authorization information can be passed electronically directly from the provider to payer, allowing you to capture more time and revenue.
Request a demo to see how you can fully automate and streamline your prior authorization workflow using the Infinx Patient Access Software solution. Contact us at [email protected].