White Paper
The Essential Guide to Prior Authorizations
Executive Summary
As scientific advancements become more commonplace in today’s healthcare environment, providers are suffocating under the insurance-mandated prior authorization requirements for advanced testing and procedures. With access to AI-enhanced software with machine learning capabilities that expertly navigate the prior authorization landscape, healthcare providers can harness bi-directional, integrated technology. Prior authorizations are now identified, optimized, and submitted, with follow-up streamlined and final approval attained in real-time. Today’s healthcare providers have the proven ability to increase revenue while significantly reducing administrative costs.
Artificial Intelligence is Ushering in Massive Change for the Healthcare Industry
The growing use of artificial intelligence (AI) technology in the healthcare industry brings new and exacting ways to support the clinical decision process, as examples:

- Advanced identification in imaging studies for radiology
- Surgical robotics in specialties like cardiology and orthopedics
- Sleep apnea detection in sleep medicine
- Analyzing bacterial colony morphology in laboratory testing
AI and machine learning is having positive results in the patient care arena.
Simultaneously, AI is being introduced into the healthcare business lifecycle through patient access and revenue cycle management (RCM) to enhance collectible revenue, reduce claim denials and rejections, and bring far less burdensome administrative worklows. The ultimate winner in this evolution is undoubtedly the patient experience.

Offering a disruptive opportunity to revisit and transform the way we do business, automation, and AI-driven technology brings both apprehension and enthusiasm in equal parts. As we imagine the possibilities, there is a sense of trepidation that artificial intelligence will replace jobs and make human intellect obsolete. However, on the flip side, few advances have offered such massive reimbursement opportunities to patients, providers, ancillary entities, and insurance payers at the same time.
Two Major Systemic Shifts in Healthcare that are Impacting Overall Delivery
High Tech Diagnosis and Treatment Options Grow
While traditional diagnostic, treatment, and care delivery techniques have been the foundation of clinical practice, every specialty of medicine is presented with new and technologically advanced opportunities that raise the bar on their ability to provide state-of-the-art care
As an example, molecular and genetic diagnostics in laboratory testing are becoming rising stars with new and better tests developed every day. Today, molecular and genetic testing is responsible for an estimated $8.7 billion in laboratory revenue and is expected to grow to $12.9 billion in 2024.
Growing at a similar pace is the field of advanced imaging, including studies utilizing CT and PET scans, nuclear medicine, and MRIs, that continues to expand in use. Their importance as diagnostic tools is ever-expanding and considered an essential “standard of care” in a growing number of situations.
An Aging Population Transforms the Procedure Mix Industry-Wide
In addition to the expanding repertoire of advanced testing and procedures brought about by forwarding leaps in technology, our population is healthier and living longer than at any other time in history. With this comes an increase to age-related deterioration issues such as osteoarthritis that impacts orthopedic replacement procedures, including knee and hip replacement surgery and the related rehabilitation, age-related cardiovascular disease, sleep apnea, and sleep-related disorders, and cancer propensities that increase with age, i.e., colon, breast, prostate.
The Growing Reimbursement Dilemma
This creates a healthcare reimbursement conundrum that is growing exponentially unmanageable. Providers, seeking to improve patient care and outcomes, are finding more opportunities to use advanced testing in their diagnostic process, and face a patient base needing more age-related care. This, in turn, creates growing problems for insurance payers who are trying to contain costs and ensure medically sound and appropriate patient care is being delivered.
Prior Authorization — Insurance Payers’ Tool of Choice
To balance the expanding diagnostic testing choices and advanced procedure options with existing levels of contractual obligation, insurance payers are using prior authorizations as a way to manage physician behaviors and patient expectations. With younger clinicians entering the system that wants increasingly advanced diagnostics and treatment options, the use of prior authorizations will become more, not less, prevalent.


CLIENT: Highly successful east coast outpatient radiology group with a large medical imaging center specializing in full major modality scans, specifically CT, PET, MRI, and Nuclear Medicine.
CHALLENGE: Experiencing an overwhelming volume of prior authorization demands from referring providers (>70%), Infinx implemented a scalable solution offering total automation of the prior authorization workflow, an intuitive interface with a cloud-based access, and expedited support for emergent requests.
RESULTS: The client saw the following results in less than two months:
- Faster turnaround time for prior authorizations and expedited scheduling
- Increased revenue by $750-$1,000 per day
- Reduced patient migration with more competitive prior authorizations by 30% per day
- Significantly reduced manual tasks and administrative time
- Strengthened relations with referring providers and practices
Industry-Wide Pressure from Prior Authorizations
Healthcare providers, whether hospital or practice-based, continue to experience the administrative burdens placed on them by increasing prior authorization obligations. In the macro sense, the industry continues to absorb an aging population that’s living longer and requires more care, the increasing use of High Deductible Healthcare Plans (HDHP) that transfer additional costs to patients, and the perpetual decline in reimbursement due to, among other things, the Protecting Access to Medicare Act of 2014 (PAMA).
Originally conceived and developed as a utilization review technique in the last century, prior authorization mandates issued by insurance payers have evolved into a time-consuming administrative burden that negatively impacts revenue for hospitals and providers system-wide. Creating adverse consequences throughout healthcare, far-reaching implications are detailed in the American Medical Association’s (AMA) 2018 Prior Authorization Physician Survey where 91% of respondents reported care delays and 28% said that the often delayed process led to serious adverse events for patients (i.e., death, hospitalization, or a life-threatening event).


TARGET: TARGET: New England-based orthopedic specialty hospital with 90 affiliated surgeons ranked as one of the top hospitals by US News & World Report.
CHALLENGE: Facing a growing backlog that hampered patient access and stymied throughput, the average prior authorization took 11 days and resulted in frustrated physicians and patients.
RESULTS: Leveraging AI to automate and standardize the prior authorization task, made their process more reliable and scalable with bots to handle repetitive tasks and decreased turnaround times to 2.5 days with increased accuracy.
An Avoidable Pain Point in Many Groups and Practices
With an estimated 182 million prior authorization transactions processed per year according to the Medical Group Management Association (MGMA), it is easy to see where issues are bound to arise related to sheer volume. With that in mind, this fact seems almost inconceivable: prior authorizations are the least automated business function in most practices. While verifying insurance and filing claims is made electronically in many, if not most hospitals, practices, and ancillary or outpatient departments, only 13% of business departments use a fully automated prior authorization solution.
With significant reform campaigns proposed or underway through the American Medical Association11 and Congress, little change has been forthcoming, and 87% of participants industry-wide are still manually processing prior authorizations using labor-intensive methods (i.e., phone and fax) that require several hours to several weeks to complete.


CLIENT: Large multi-facility cardiology practice with 50-60 providers in Central Texas specializing in advanced cardiology and electrophysiology.
CHALLENGE: Experiencing an overwhelming volume of claims denials and rejections, Infinx was engaged to investigate root causes and determine a course of action. It was quickly determined that over 80% of the denied claims were due to missing or incomplete PAs.
RESULTS: Using the Infinx Prior Authorization Software, and automating their previously manual prior authorization system provided the following results:
- A streamlined and automated system that returned completed prior authorization in real-time
- Reduced rework and follow-up on missing prior authorizations and significantly decreased the denials and rejections received from insurance payers
- An ongoing partnership formed due to the success of the initial phase, that expanded to their entire patient access and RCM workflows
AI-Driven Technology Solves the Prior Authorization Equation
We hear a lot about AI these days and what it means to solve our most frustrating problems like reducing manual, timeconsuming, and repetitive tasks or removing human error from the prior authorization equation?
Explaining the detailed logistics of how AI works can be formidable, however, this clarification is suitable for our purposes: utilizing a predefined set of algorithms, AI-driven software uses statistical analysis to unlock data insights. It then supports data-driven decisions that improve the timeliness and accuracy of targeted outcomes. AI programming can combine large chunks of data through iterative processing allowing the software to “learn” by memorizing patterns in the data.
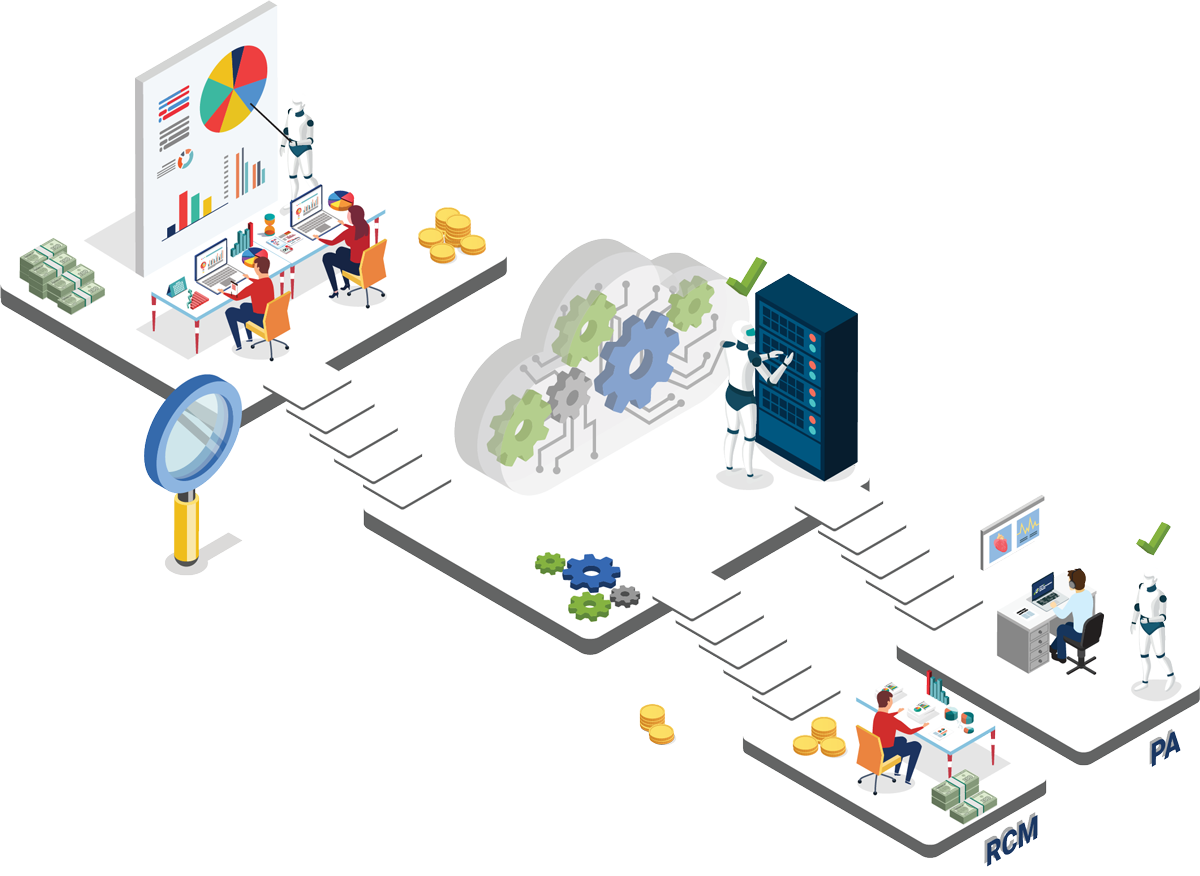
To illustrate through the lens of prior authorizations, AI-driven software would be integrated bi-directionally with a practice or group’s EHR/EMR and billing system used for client management through cloud-based technology. As a patient’s order arrives, tests or procedures requiring prior authorizations would be electronically identified, provider/facility detail, patient demographics, and test/diagnosis information would be collected, and an approval request submitted in real-time to the insurance payer through highly secure cloud technology.
To electronically determine the prior authorization parameters and route the request to the appropriate insurance payer portal, AI-driven software with machine learning capabilities would access continually updated insurance information clearinghouses storing thousands of insurance groups and plans, each with their unique guidelines and requirements. Prior authorization approvals that once took several hours to several days or weeks can now be initiated in real-tie with a 98+% accuracy rate.17

A Comprehensive and Secure Cloud-Based Solution
Infinx creates a seamless and scalable prior authorization solution that uses Health Level 7 (HL7) or Application Program Interface (API) based integration and is compatible with all leading EHR/EMR, Billing, and LIS systems. The Infinx Prior Authorization Software embeds all Patient Health Information (PHI) in layers of security: Electronic Data Interchange (EDI) compliant and stores the data on the cloud using 64-bit and 256-bit encryption that guarantees 100% HIPAA compliance.
An Automated Solution to the Inevitable Prior Authorization Follow-Up, Appeals, and Changes
No longer relying on manual workflow, prior authorizations can be tracked using real-time analytics, followed up electronically 24/7, with the status continually updated on an interactive dashboard. When appeals are needed, customized solutions can be defined, and the system can seamlessly execute their protocols. This eliminates the need for personnel to spend countless hours on hold or faxing information to the myriad insurance payers, each with their own set of guidelines.
AI Supported by Human Intelligence
By itself, automation and AI-driven software is capable of amazing things. However, to have a truly comprehensive prior authorization process, one must have a support team of highly trained specialists available to supplement with human intelligence and problem-solving skills. When emergent or complex requests and exceptions arise, it will be through a team of trained specialists that an organization is ensured complete coverage for their prior authorization process.


CLIENT: Prominent San Francisco area clinical laboratory focusing on prenatal genetic screening and seeking an innovative solution before ramping up nationwide production.
CHALLENGE: Ramping up their prenatal and carrier screenings program for female patients during their ninth week of pregnancy, the client was searching for a third-party partner that would provide the technical expertise, training, and support to expand their prior authorization program.
RESULTS: Using the Infinx Prior Authorization Software, and automating their previously manual prior authorization system provided the following results:
- Designed and implemented an automated system that was scalable and highly accurate
- Quadrupled prior authorization volume during the pilot phase of the project
- Improved the overall prior authorization accuracy rate from 65% to 98% upon implementation
- Delivered 100% compliance with all payer guidelines and protocols
- Conducted audits for quality based on agreed-upon metrics and continued to optimize operations as part of an ongoing partnership

Enjoy Increased Revenue Through Automated Workflow
The prior authorization process is the least appreciated function in any hospital, practice, or facility. It is rightfully seen as disruptive to the patient’s care and experience, a roadblock to necessary procedures and equipment, and uncompensated use of physician and staff time.

While the field of sleep medicine is expanding, there are specific categories of therapy, testing, and supplies that routinely require prior authorization, including:
- Polysomnography; sleep staging and staging with the initiation of continuous positive airway pressure therapy (CPAP) or bilevel ventilation, attended by a technologist
- Home sleep apnea testing
- Use of durable medical equipment, including respiratory assist devices, bi-level pressure and humidifier components
- Delivered 100% compliance with all payer guidelines and protocols
- Corresponding supplies, such as full-face, and nasal masks, headgear, chinstraps
Without timely and accurate prior authorizations, these services are at risk of being denied and the patient being responsible at 100%.
Now, more than ever, healthcare is under unrelenting financial pressure — from changes to payment models and fee schedules to ever-reducing reimbursement structures, revenue is, at best, holding steady or, at worst, steadily falling industrywide. With a future that promises improving healthcare outcomes reliant on more and better diagnostic tools and improved medical procedures and techniques, everyone is finding themselves in a financial vice grip that’s only going to get worse.
One way to make a substantial impact is to use automation and AI to accelerate the prior authorization approvals With automated prior authorizations, the opportunity to positively impact revenue is three-fold:
1. Stop patient abandonment of care through quickly completed prior authorizations that allow immediate scheduling and care progression
2. Reduce claim denials and rejections by as much as 80%
3. Redirect staff costs to higher-value functions including improving the patient’s overall experience and retention
The 2019 CAQH Index, a widely-respected bellwether, recently released estimates that the current cost to process a prior authorization is estimated to be $14.24 (manual) vs. $1.93 (electronic) at a potential industry-wide savings of $12.31 for each occurrence. While their methodology uses a lot of variables, like salary costs, insurance company variants, and procedure/test mix that can vary from region to region, the cost savings are significant and worth consideration.

What the Future Holds
One’s imagination only limits the future for AI in healthcare. Certainly, in the near term, AI-supported functionality in the healthcare billing lifecycle will evolve into a richer and more comprehensive ability to evaluate clinical details to ensure medical necessity for prior authorizations before they are submitted for approval.
Further improving the patient experience will be advances in the patient access area with improvements that will facilitate scheduling and managing the patient’s propensity to pay. As well, AI is supportive in the new Clinical Decision Support Mechanism (CDSM) process that impacts not only radiologists but also any primary or specialty care providers that order advanced imaging procedures for Medicare patients.
In fact, recognizing the challenges brought by the new CDSM, the Centers for Medicare and Medicaid Services (CMS) extended the mandatory implementation date to January 1, 2022 This extension is intended to give both ordering and furnishing providers ample time to negotiate the technological and workflow challenges before there is a monetary impact.
In Summary
Taking the macro view, we see an industry in flux and under the most stringent constraints in reimbursement reduction, increasing paperwork, and administrative headaches. This is causing industry-wide clinician and provider burnout at unprecedented rates. By continuing to create an unsatisfying environment, coupled with rising population growth and an increasing number of seniors seeking care, we’re projected to experience an estimated 120,000 physician shortfall by 2030.
To date, legislative relief has not produced any tangible results in combating the prior authorization problem. Simultaneously, numerous healthcare-related entities (including some insurance payer associations) have thrown their collective weight at the problem and have been rebuked.
A more proactive stance would be to embrace the paradigm-shifting technology of automation and AI-driven software. Coupled with highly trained specialists for outliers, hospitals, providers, and groups can recognize substantial cost savings through decreasing workloads, significantly reducing denials and AR rework, and improved revenue capture.
About Infinx
Infinx provides innovative and scalable payment lifecycle solutions for healthcare practices. Combining an intelligent, cloud-based platform driven by artificial intelligence and automation, with our trained and certified prior authorization, coding and billing specialists, we help clients realize revenue, enabling them to shift focus from administrative details to billable patient care.