Powered by AI, automation & revenue cycle expertise
We provide a comprehensive approach to patient access and revenue cycle management by combining advanced automation, AI-powered workflows, and experienced specialists. Our solutions are designed to address the unique challenges of RCM, including:
- Leveraging AI for tasks requiring reasoning and decision-making, such as prior authorizations and clinical documentation reviews.
- Automating routine workflows like eligibility verification, claims tracking, and payment posting.
- Supporting complex processes like claims resolution and patient engagement with expert human intervention.
With seamless integration into leading EHR and billing systems, our solutions simplify workflows, reduce costs, and improve financial outcomes.
Gen AI / ML / NLP

Intelligent Automation & RPA

Predictive Analytics Insights
HL7/API/RPA EHR Integrations

Payer/TPA Integrations
Billions of transactions processed. Decades of experience.
Our advanced technology and expert team have processed billions of transactions for leading healthcare organizations from 1,400+ payers nationwide. With deep experience across patient access and revenue cycle workflows, we help providers achieve better outcomes at scale.
4000+
Facilities Served
5M+
Patients Served
$8B+
Revenue Collected
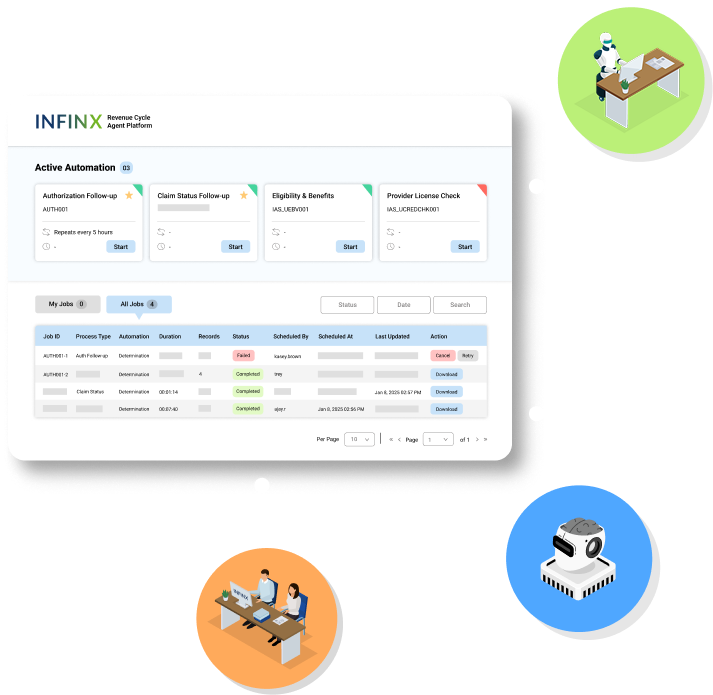
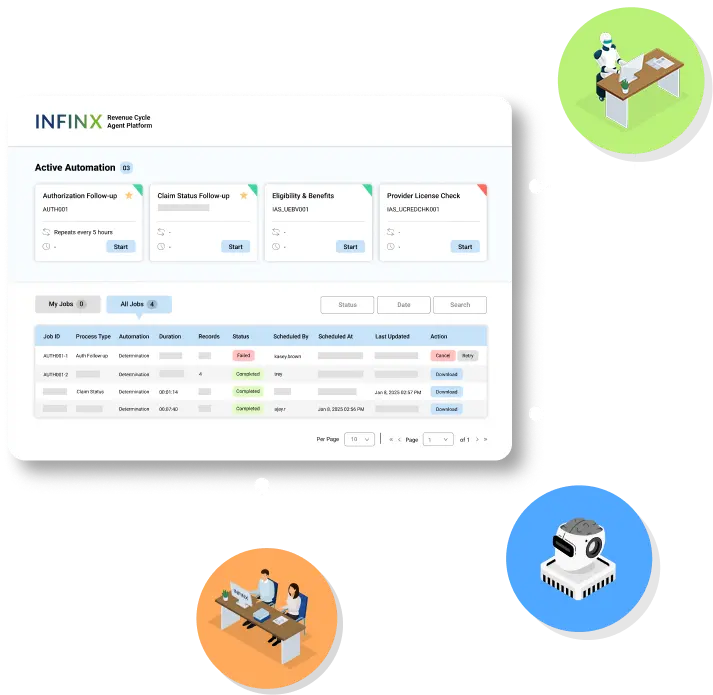
REVENUE CYCLE AGENT PLATFORM
AI, automation, and human agents working together for better RCM outcomes
We’ve continuously leveraged AI, automation, and human specialists in our revenue cycle solutions. Our Revenue Cycle Agent Platform makes these intelligent agents available as a standalone, modular solution, seamlessly integrating into existing systems. With our Healthcare Revenue Cloud technology ecosystem as its foundation, this multi-agent approach brings intelligence, precision, and expertise to RCM processes.
- AI agents handle complex reasoning plus action workflows
- Automation agents handle high-volume, repetitive workflows
- Human agent specialists step in where expertise and manual intervention are required
- HL7/API/RPA interoperability with EHRs
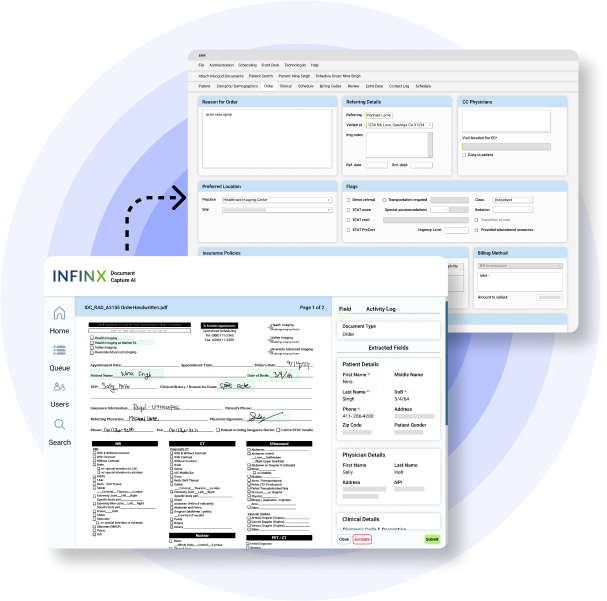
DOCUMENT CAPTURE AI PLATFORM
Smarter, faster document processing developed specifically for healthcare providers
Powered by our AI, automation and human agents, our Document Capture AI platform goes beyond OCR by automatically classifying, extracting, and validating data for completeness. Extracted patient data flows directly from intake to EHR in real-time and automating next-step actions, such as creating new orders or updating prior authorizations.
- Document classification AI agent
- Context aware data extraction AI agent
- Validation, error detection & queue management
- Human-in-the-loop intevention for review and auditing
- Automated actions in EHR
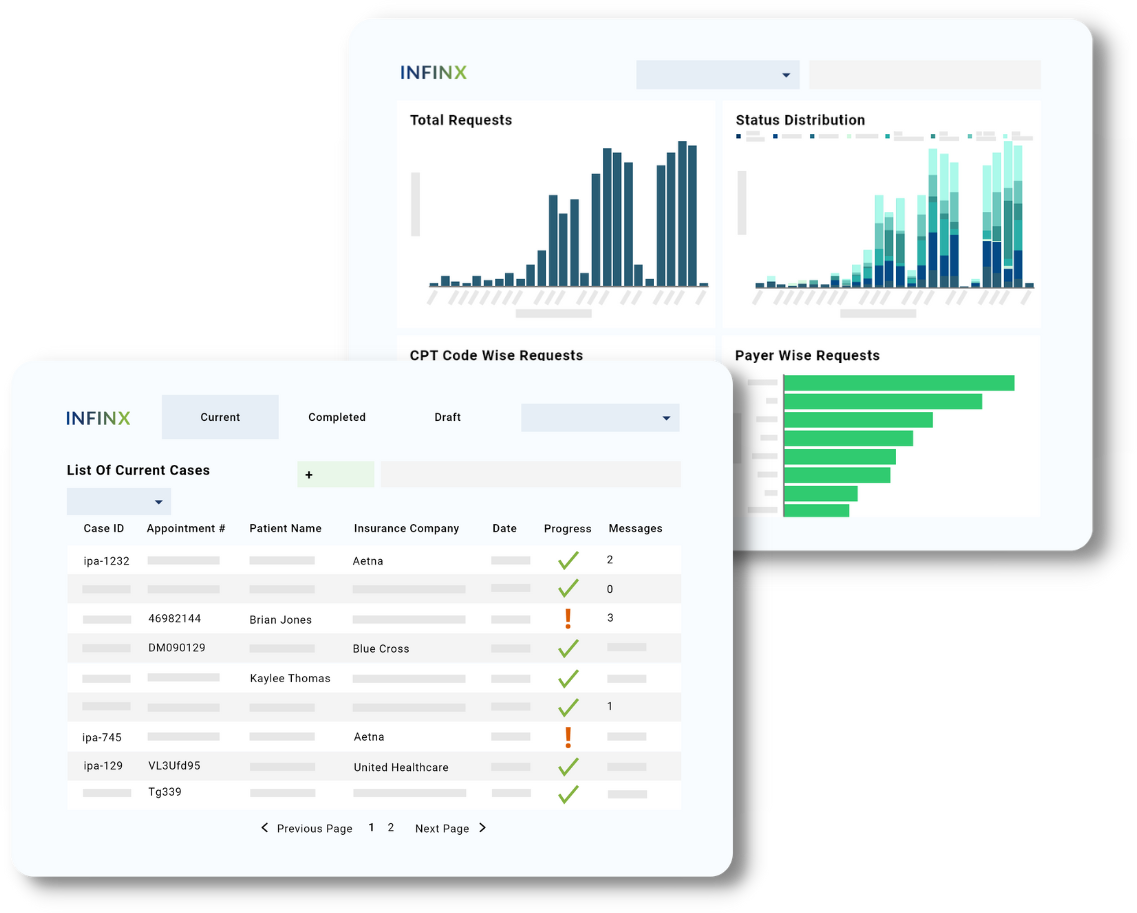
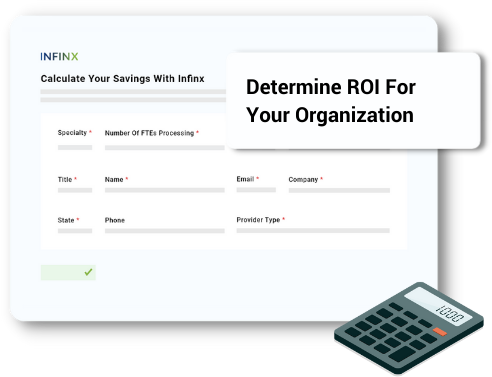
PATIENT ACCESS PLUS
Faster eligibility verifications, benefits checks and prior authorizations
Get quicker financial clearance for patients before care with our Patient Access Plus platform that provides complete coverage for obtaining eligibility verifications, benefit checks, patient pay estimates and prior authorization approvals, all in one system.
- HL7/FHIR/API Integration
- Automation Agents
- Workflow Management
- Payer/Clearinghouse Integration
- ML/AI Execution
- Analytics Dashboard
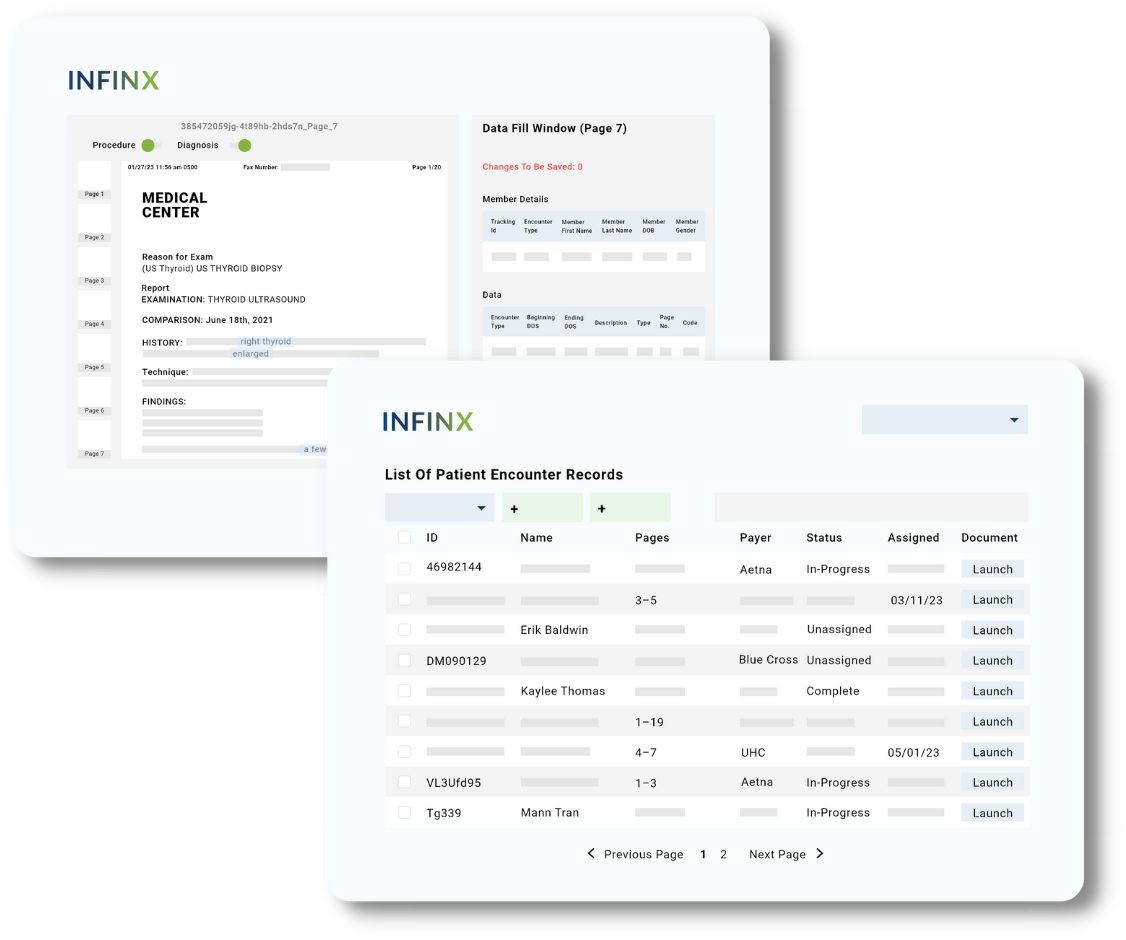
HIM & CODING
Increase clean claim submission and reduce coding-related denials
Convert patient care to maximum recoverable revenue by ensuring accurate claims are submitted the first time around leveraging automation, AI, certified coders, billing specialists and payer compliance experts.
- Certified & Specialty Coders
- HL7/FHIR/API Integration
- ML/AI/NLP Execution
- Workflow Management
- Denial Analytics
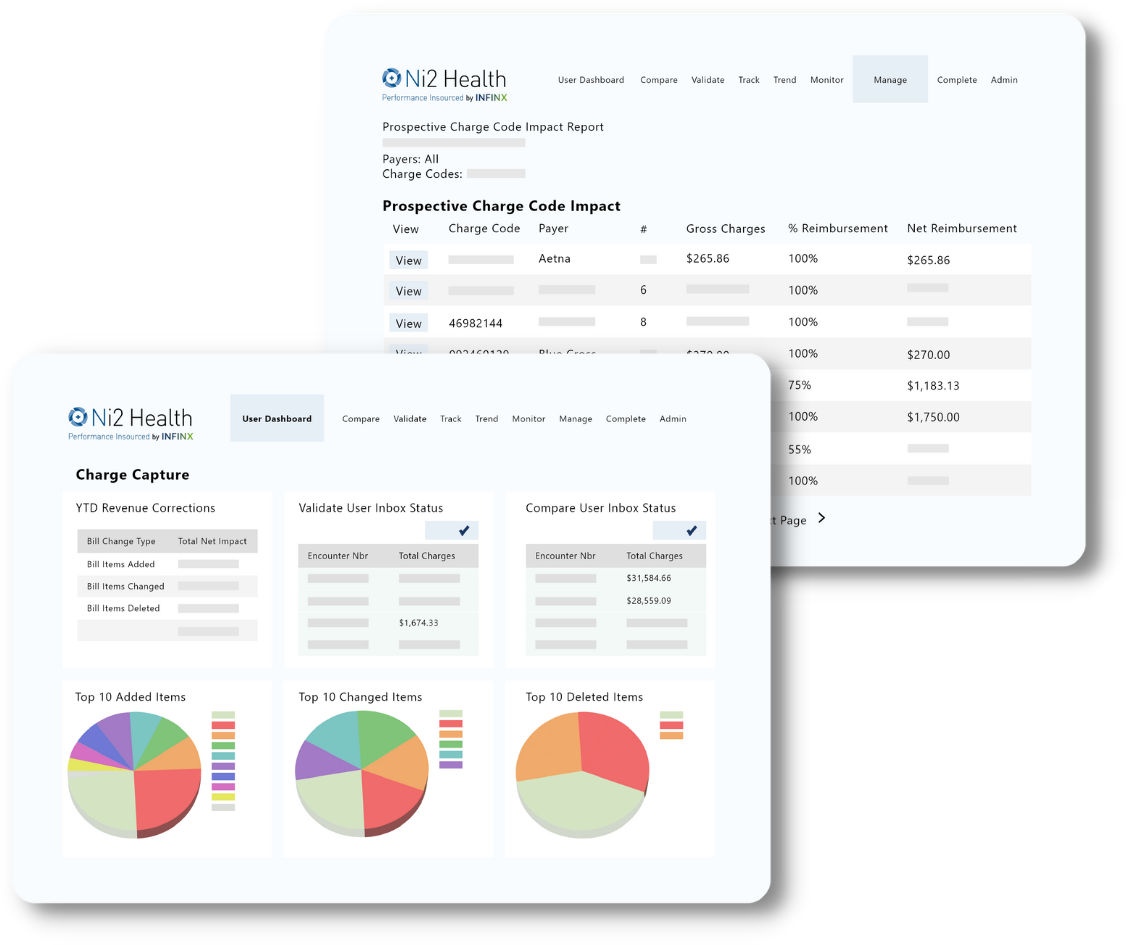
REVENUE INTEGRITY
Optimize charge capture workflows
Convert patient care to maximum recoverable revenue by ensuring complete and accurate charge capture covers patient care delivered are submitted the first time around leveraging automation, AI, certified coders, billing specialists and payer compliance experts.
- Charge Capture Technology
- AI/ML/RPA Execution
- HL7/FHIR/API Integration
- Workflow Management
- Denials Analytics
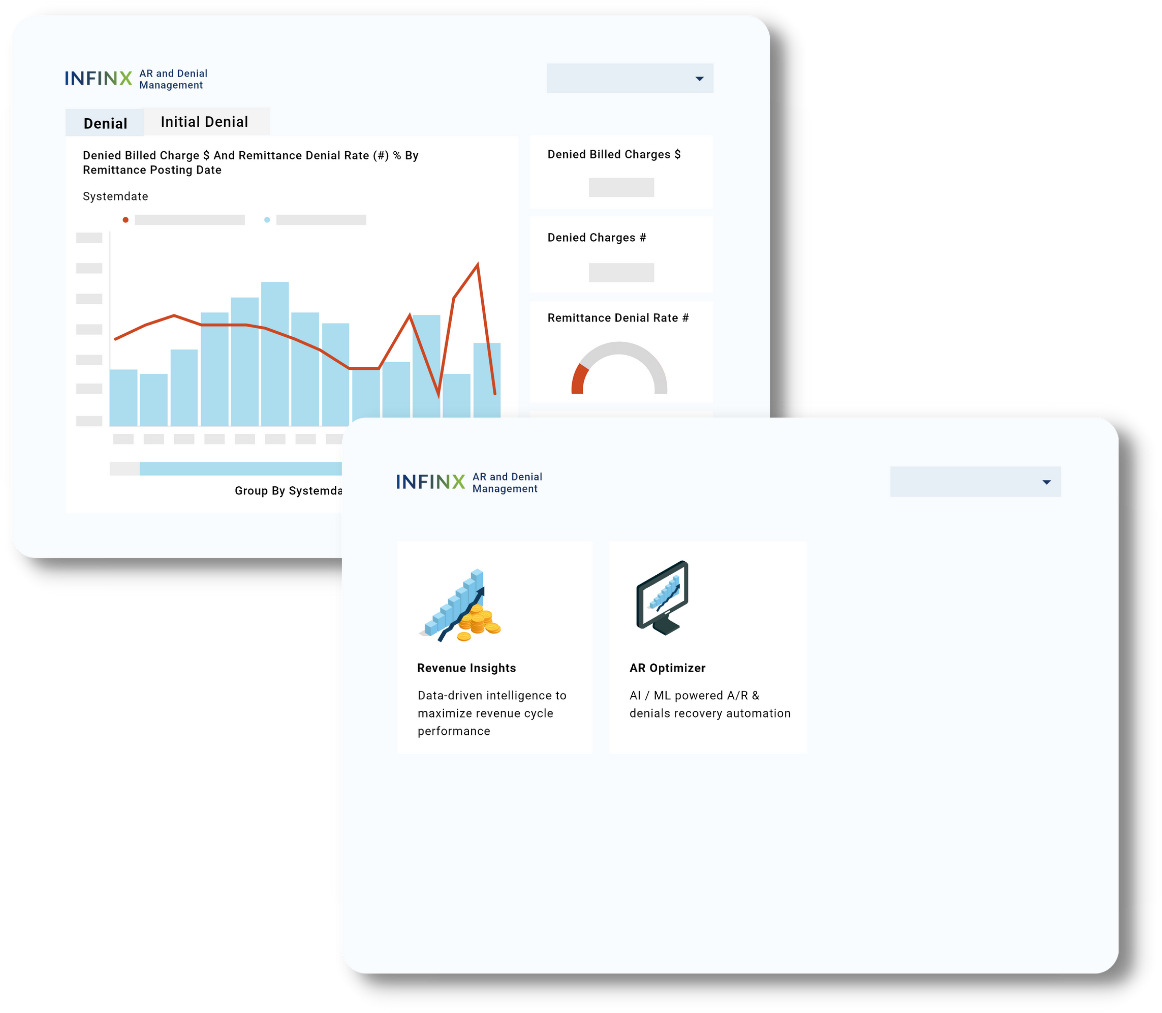
A/R RECOVERY & DENIALS MANAGEMENT (ARDM)
Predict recovery, prioritize A/R & denial claims follow-up
Maximize reimbursements from A/R inventory and denied claims, as well as reduce future denials with our A/R Recovery & Denials Management platform, powered by AI, automation, intelligent workflow management, predictive analytics and billing specialists.
- AI/ML Execution
- Automation Agents
- Advanced Predictive Analytics
- HL7/FHIR/API Integration
- Payer/Clearinghouse Integration
- Workflow Management
Integrations
Compatible with most healthcare software systems
We offer bi-directional integration with most systems with API, HL7, FHIR, X12 or EMR developer programs so that your staff can continue to work in their local system. Here are some of the systems we integrate or are compatible with. Epic is a registered trademark of Epic Systems Corporation.










Recognized as a trusted technology partner
We have been recognized by Gartner, KLAS and Black Book Research as a vendor who can help providers and payers automate their patient access and revenue cycle workflows.
We’d like to help change that
Our mission is to automate and make patient access and revenue cycle workflows more intelligent where possible so that our client providers and staff can focus on high-value work like growing their business and keeping their patients healthy and happy.
Technology adoption in healthcare is challenging
While AI, machine learning and robotic process automation in other industries have been widely implemented, the healthcare industry as a whole has been slow to adopt these innovative technologies to make revenue cycle management more efficient due to non-standard processes and legacy systems.
How We Help Reduce The Revenue Cycle Bottleneck
By offering a complete and scalable solution of technology + experts, we are able to increase prior authorization approvals, reduce claim denials and clear aged A/R, thereby significantly impacting our client provider’s bottom line.
SPECIALTIES
Our clinical expertise
Given our years of experience, we have helped many specialty hospitals, ASCs and physician groups streamline their patient access and revenue cycle workflows. Even if you don’t see your specialty below, please don’t hesitate to contact us.
Behavioral Health
Cardiology
Dental

DME

ENT

Gastroenterology
Hospital
Laboratory
LTC Pharmacy
OBGYN

Oncology
Ophthamalogy
Orthopedic
Pain
Radiology/Imaging
Rheumatology
Rural Hospital

Specialty Pharmacy
Speech Therapy
Therapy
Urology
Wound Care
We love helping our clients optimize their reimbursement workflow
“We have cut 50% of our costs with Infinx. Now there are no appointment cancellations. Our urgent prior authorization requests are processed on time and our physicians no longer have to manage insurance companies.”
Executive Vice President
National Radiology Group
“Since adopting Infinx’s platform, we’ve seen a 90% decrease in workload on our team, and a 2% denial rate. We’re actually spending a lot more time with patients.”
Patient Access Director
Radiology Group in Florida
“I oversee coding, billing, and other functions. Working with Infinx, we have been able to maintain our costs while getting resources quickly. Infinx staff are trained and experienced and work well with our staff. They have become our RCM partner.”
HIMS Director
Hospital in Texas
Find more time for high-value patient care
With our complete tech + specialists solution, our client providers have been able to focus more on patient care.
30% Reduction in 120+ days aged A/R inventory.
20% Improvement in utilization due to real time authorization determination.
20% Average reduction in days in A/R.
98+% Coding accuracy leading to reduced denials and timely collections.
60% Reduction in cost to collect.
14% Increase in net collection ratio (NCR).
Patient satisfaction, priceless
We partner with leading brands
Collaboration without borders
7,200+ Employees
Empowering Innovation
Joining forces globally to transform US healthcare workflows.
3 Countries
Global Footprint
Key operations in the USA, India, and the Philippines, focused on delivering world-class solutions for the US healthcare market.
AI-Driven
Advanced Technology
Using AI and automation to enhance revenue cycle management.
24/7
Around-the-Clock Support
Ensuring seamless service delivery from teams across the globe.