PRIOR AUTHORIZATION SUPPORT
We Help Your Referring Physicians Obtain Authorization Approvals
For some procedures, payers and benefit managers do not accept prior authorizations initiated by rendering providers. If the referring physician does not have capability in place to quickly process authorization requests, this can impact your ability to schedule services efficiently.
Referring physicians become approved users of your subscription
We help remove this bottleneck by making it easy for referring physicians to become approved users on your Patient Access Plus subscription so they can leverage our solution and expertise to quickly obtain prior authorization approvals during the referral process.
Schedule more services and reduce denials downstream
By making it easier for physicians to send patients with authorizations already approved, your staff will be able to schedule more services, and claims downstream will have a lesser likelihood of getting denied due to any prior authorization issue.
HOW IT WORKS
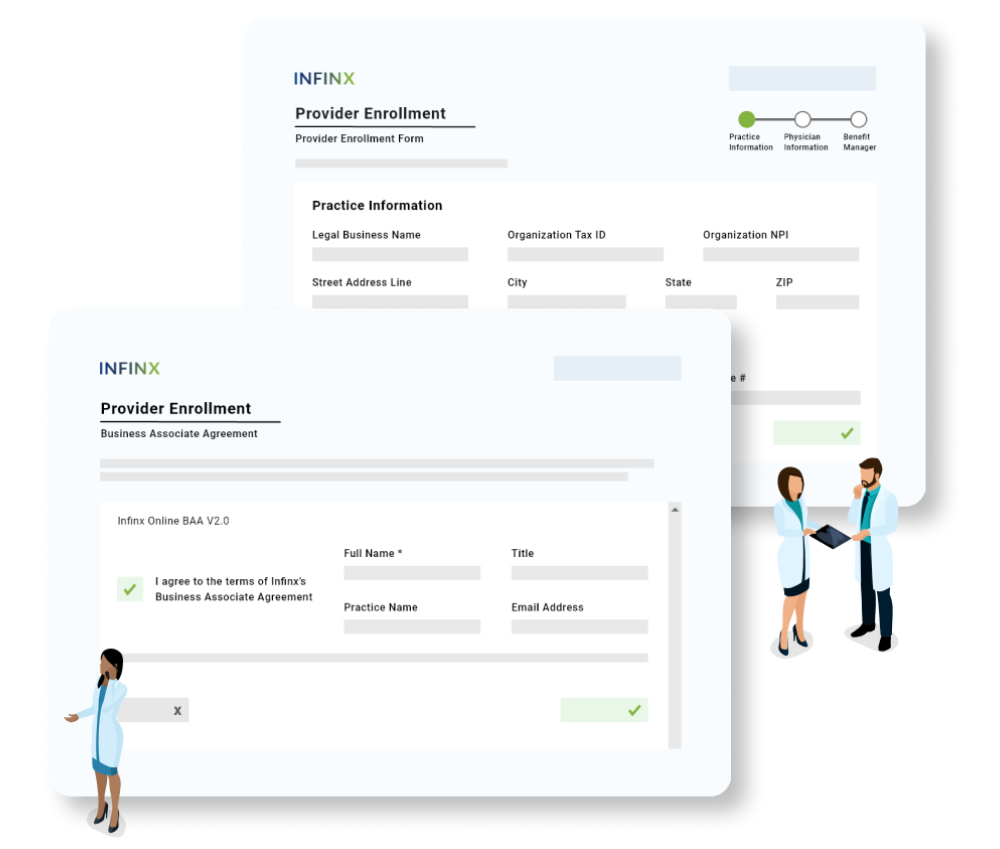
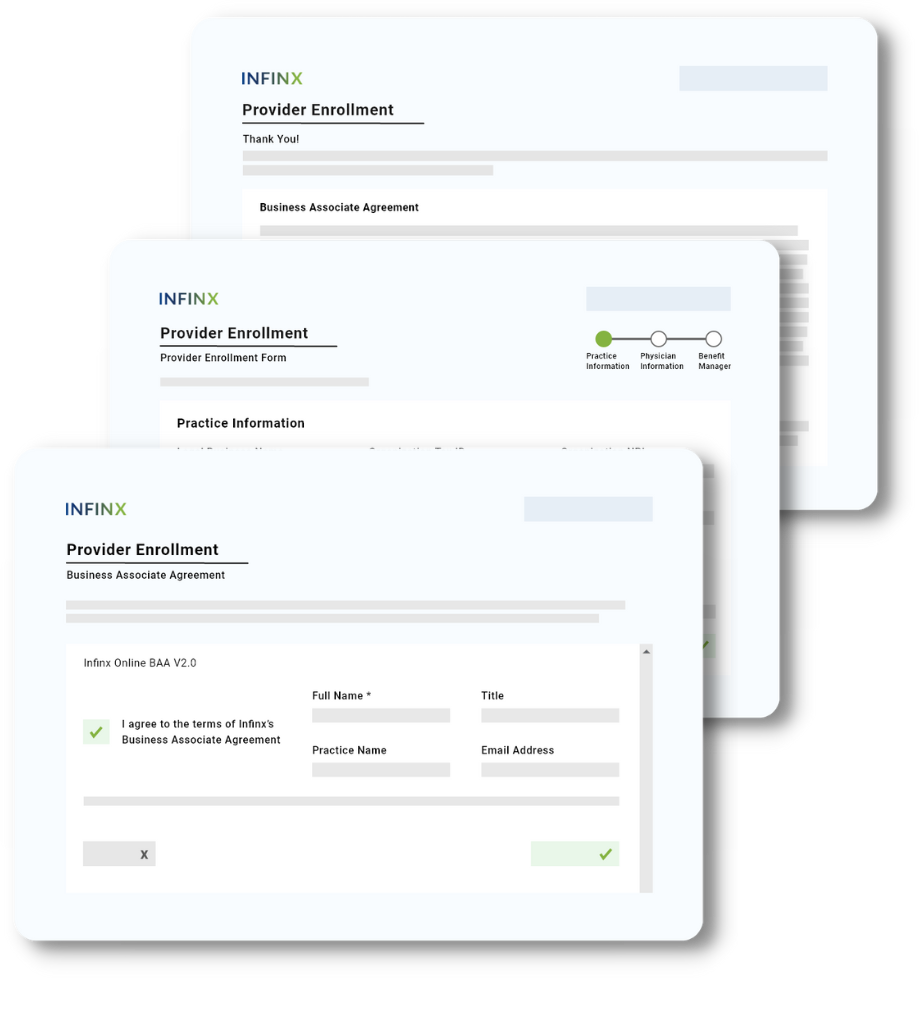
Easy Onboarding Steps For Providers
Our easy workflow is designed to help referring physicians with little or no prior authorization experience. Referring providers sign our online Provider Enrollment form and Business Associate Agreement (BAA). We create benefit manager credentials on their behalf. When your referring physicians are successfully enrolled, orders can be submitted and we will help obtain prior authorization approvals.

Introduction
Introduce Infinx to referring physicians with flyer and custom web page.

Completes Form
Referring physician signs our provider enrollment form and BAA.

Credentials Created
Benefit manager credentials are created on referring physician’s behalf.

Prior Auth Permissions Granted
Infinx is permitted to process prior auth requests in client’s Patient Access Plus.

PRIOR AUTHORIZATION COLLATERAL
Educate Your Referring Physicians With Marketing Support
We partner with our client providers to provide everything they need to roll out a comprehensive program out to their referring providers, including:
- Co-branded sign up page for referring physicians
- Co-branded marketing flyers to gain physician participation
- Custom provider enrollment landing page to direct referring providers to along with an overview and instructions on how to enroll electronically
- Confirmation emails sent upon enrollment by referring providers

COMPLETE COVERAGE
Ensures Prior Authorization Approvals For All Orders
Our processes are designed to work with hospitals and physician groups with little to no prior authorization experience. We successfully obtain prior authorizations across a wide variety of specialty areas including cardiology, orthopedics, oncology, gynecology, neurology, gastroenterology, and more each day.