PATIENT ACCESS PLUS
Streamlined prior authorizations, powered by the latest tech
Navigating prior authorization processes can be tedious and time-consuming, leading to delays in patient care and operational inefficiencies. We optimize the way healthcare providers handle prior authorizations with our AI-powered platform, Patient Access Plus.
Our solutions are tailored to your existing workflows and are designed to deliver accuracy, speed, and scalability, ensuring that providers can focus on delivering exceptional patient care.
POWERED BY AI, AUTOMATION, SMART WORKFLOWS & DOMAIN EXPERTISE
Customized platform available for your unique needs
With Patient Access Plus, you can rely on the same patient and service details inputs to trigger prior authorization workflows that are optimized with AI, automation, intelligent workflow management and support from our in-house team of specialists. We also set up custom platforms armed with automation agents for various use cases to help providers reduce repetitive work performed by their staff so they can focus more on engaging with their patients.
Clients are able to refer to the same dashboard for eligibility verifications, benefit checks, patient out-of-pocket estimations, insurance discovery, prior authorization requests and CDSM consults.
SOFTWARE ONLY
Patient Access
Your team leverages our technology to perform automated patient access activities where possible before scheduling patients.
- Prior authorization
- Eligibility verifications
- Expanded plan & procedure benefits view
- Patient pay estimates
- Insurance discovery pre-service
- Patient access analytics
- Full service support by Infinx team
- CDSM
SOFTWARE + OUR SPECIALISTS
Patient Access Plus
We provide complete coverage where our specialists leverages our technology to manage patient access checks for your organization. CDSM consult module can be added upon request.
- Prior Authorizations
- Eligibility verifications
- Expanded plan & procedure benefits view
- Patient pay estimates
- Insurance discovery pre-service
- Patient access analytics
- Full service support by Infinx team
- CDSM
AUTOMATION AGENTS
Automate Prior Authorization Tasks
Reduce hours spent by staff on mundane tasks in the patient access workflow. Automation agents tackling various use cases custom built for your organization.
- Initiate prior authorization request
- Electronically submit request to payer
- Check payer portal for status updates
- Post updates to EMR
- Repeated follow-up with payers
- Initiate eligibility verification
- Initiate benefit checks
- Initiate insurance discovery
- and other patient access tasks
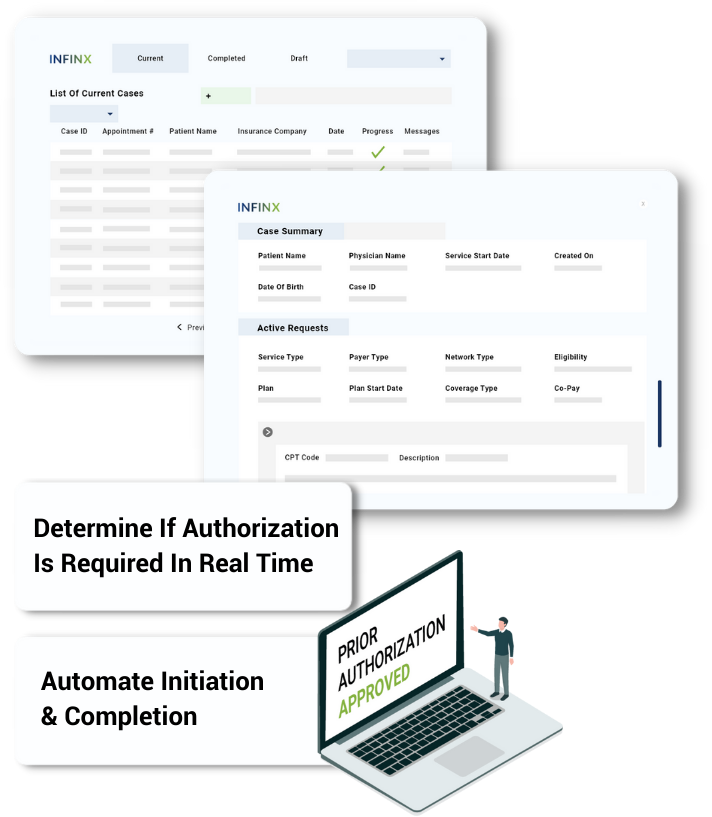
AUTHORIZATION DETERMINATION ENGINE
Shortlist which cases need authorization instantly
Leverage AI and extensive integrations for clearinghouses and benefit managers to check if prior authorization approvals are required to care.
Determines if prior authorization is required
Our authorization determination engine automatically determines if a prior authorization is required or not with over 98% accuracy by referring to the payer guidelines and CPT code of the service.
Learn instantly when no authorization is required
If our determination engine determines if authorization is not required, status is updated instantly in your EMR, and your staff is notified immediately.
Schedule more appointments and save hours
This feature alone has helped our clients schedule more procedures and save their staff hours spent manually reviewing payer guidelines to figure out whether authorization is required.
ELECTRONIC AUTHORIZATION SUBMISSIONS
Automate initiation, checks & updates
Initiate and submit request electronically
If an authorization is required for the service, the case is electronically submitted to the appropriate payer.
If electronic submissions not possible, case is worked manually
Complex requests and submissions to payers who do not accept electronic submissions and require manual intervention can be handled by your team or assigned to our specialists for further processing.
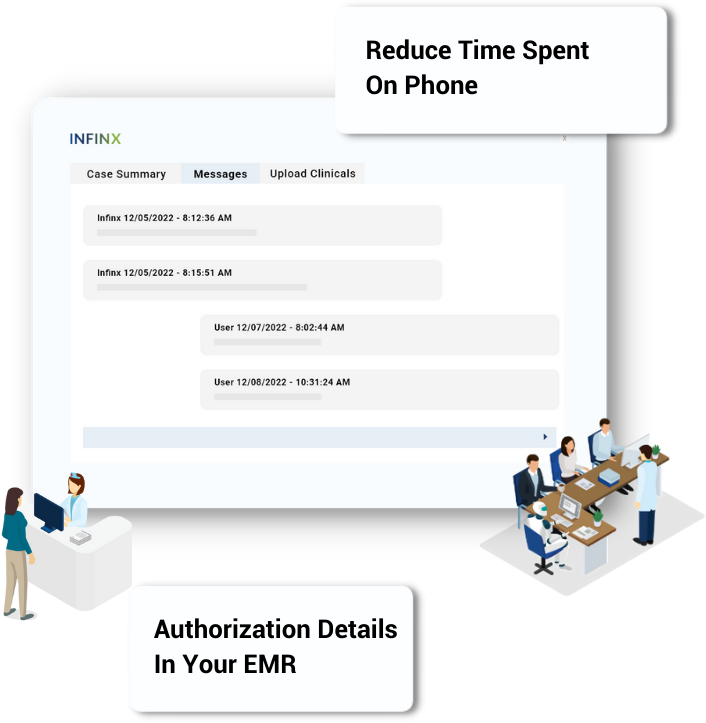
Automated status checks & updates
Automated repeated follow-up with payers and real-time status updates are provided by our automation agents. Real-time status updates help your staff keep patients informed and procedures get scheduled on time.
Your EMR updated
Once request is approved, the authorization approval package can be automatically sent back to your EMR and displayed in our web portal as well.
OUR SOFTWARE + OUR SPECIALISTS = COMPLETE COVERAGE
We take care of each prior authorization request for you
While AI and payer automations are making significant strides in optimizing revenue cycle management workflows, there is still a need for experienced team members to manually handle cases that automation cannot handle on its own or if the provider’s staffing challenges are causing backlog in critical revenue cycle tasks.
We offer a hybrid approach which is particularly beneficial for enterprise healthcare providers, like hospital systems or large outpatient groups, who:
- are not looking to completely outsource their prior authorization activities and want their teams to continue working on their cases while utilizing our proprietary technology, as well as
- desire the flexibility to easily assign a subset of their case inventory to Infinx’s specialists to work on if the need arises.
Clients rely on Infinx on as a trusted partner to manage the entire patient access workflow due to our effective and reliable team members who support them.
Specialists & Agents
Leverage our technology to perform the required patient access tasks.
Customer Success Managers
Ensure our solution works for you at every step with responsive communication and on-demand problem solving.
Technology Solution Experts
Get rapid data transfers, custom fields, EMR integration and more without extensive IT infrastructure on your end.
Senior Executives
Leverage their expertise to optimize revenue cycle workflows and outcomes at your organization and help you grow.
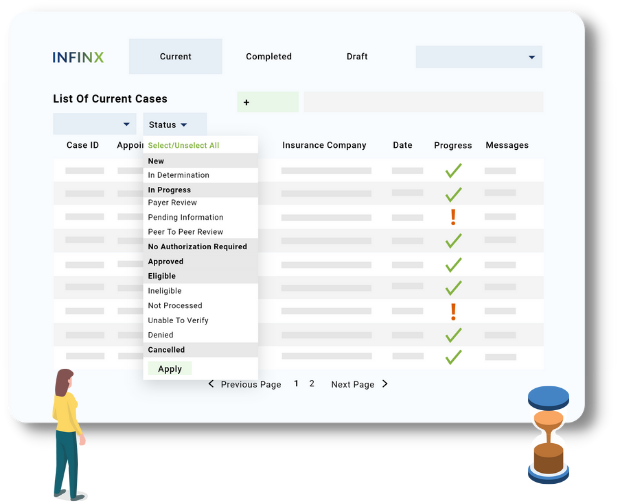
INTUITIVE DASHBOARD
Create new cases & assess status quickly
If you are accessing the Patient Access Plus web portal, our simple dashboard enables your staff to easily create new cases, and sort through the cases intuitively with the help of several filters, search and sort options.
- Product type: Eligibility & Benefits, Prior Authorization or both
- Progress status: No Authorization Required, In Progress, Action Required, Finalized, and more
- Facility Name
- Payer Name
- Date of Service
- Ordering Physician
- Case ID
When you subscribe to our solution, you’ll get access to product demo videos on how to execute each action, a user guide which is updated regularly and a dedicated customer success manager who will help you get the most benefit out of our solution.
CONTINUOUS MACHINE LEARNING
Prior authorization processing becomes easier over time
Our machine learning algorithms continues to learn from your unique data and becomes smarter and quicker as more of your prior authorization requests get processed. Here are some of the factors and results we look out for.
- Determine the need for a prior authorization
- Identify clinical requirements for a procedure
- Identify risks of denial or peer review
- Accurately predicts turnaround time
- Respond to clinical requirements
- Identify gaps in documentation
- Follow up regularly for updates
We continue to innovate our technology and optimize our workflows so your staff don’t have to worry about processing prior authorization requests any longer.
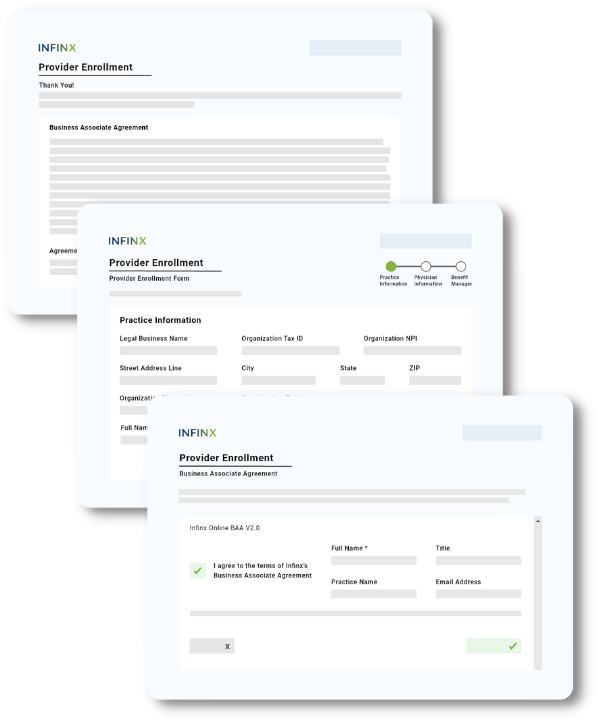
REFERRING PROVIDER REQUESTS SUPPORTED
We help your referring physicians obtain authorization approvals
For some procedures, payers and benefit managers do not accept prior authorizations initiated by rendering providers. If the referring physician does not have capability in place to quickly process authorization requests, this can impact your ability to schedule services efficiently.
Referring physicians become approved users of your subscription
We help remove this bottleneck by making it easy for referring physicians to become approved users on your Patient Access Plus subscription so they can leverage our solution and expertise to quickly obtain prior authorization approvals during the referral process.
Easy sign up process
- Referring provider signs our digital Business Associate Agreement (BAA) on a custom provider enrollment web page created just for your organization,
- Referring providers completes the Provider Enrollment form on the web page,
- Then they can easily submit prior authorizations requests to process.
Schedule more services and reduce denials downstream
By making it easier for physicians to send patients with authorizations already approved, your staff will be able to schedule more services, and claims downstream will have a lesser likelihood of getting denied due to any prior authorization issue.

PRIOR AUTHORIZATION ANALYTICS
Leverage real-time data to gain actionable authorization intelligence
Get real-time insights into your prior authorization activity with detailed and robust analytics and reporting.
Real-time comprehensive dashboard
Data gets updated in real-time. Filter reports to see the data that’s important to you
Insights to drive action
Predictive analytics insight into usage metrics to help improve your organization’s prior authorization workflow upstream and lower claim denials due to prior authorization issues downstream.
Reviews
Our clients grow with us
As we streamline their organization’s patient access workflows, clients are happy with increased results, as well as improved cash flow due to increase in reimbursements and reduction of claim denials due to eligibility. They usually end up retaining us for other revenue cycle management tasks.
“We recently reviewed our turn around times from last year to today and you can see that we are currently trending at a rate lower than last year and possibly ever before. This took a lot of hard work from Infinx and we appreciate all you do and recognize your journey to get to this point. Keep up the great work and thank you for all you do!”
Supervisor, Revenue Cycle
Publicly Traded Diagnostic Lab
“Since adopting Infinx’s platform, we’ve seen a 90% decrease in workload on our team, and a 2% denial rate. We’re actually spending a lot more time with patients.”
Patient Access Director
Radiology Group in Florida
“Infinx seamlessly processed our authorizations, even as our volume increased, without causing significant delays. By collaborating with their team, we successfully integrated our CRM and streamlined our authorization process. Communication has been excellent, and any issues we raise are thoroughly investigated and addressed with clear responses, enabling us to better serve our patients.”
Manager, Diagnostic Imaging
Hospital in Nevada
EDUCATION
Helpful resources for your team
We create educational materials frequently in the form of virtual office hours, articles, white papers, webinars and podcast episodes which help our clients and peers with common patient access challenges they face. If you would like us to address a specific topic, feel free to reach out to us.
FREE SEARCH TOOL
Search clinical guidelines for prior authorization online
Access payer policies and clinical guidelines for radiology and orthopedic procedures in seconds with our free AI-powered online search tool.
We help you identify guidelines for prior authorization and medical necessity through a simple query by procedure, payer and diagnosis.
- Policies and guidelines in our database get updated regularly to stay current
- Results provided by our AI-powered search algorithm continues to refine as the search volume increases
Search results return only the relevant guideline sections saving you time reviewing and hunting for the information.
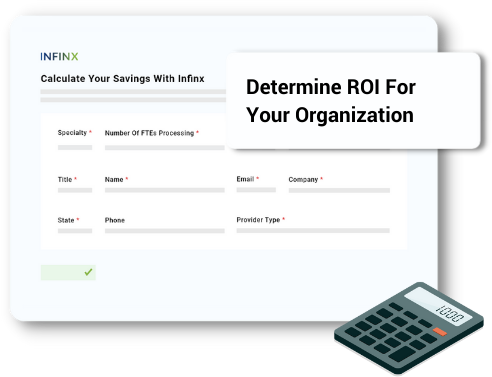
PRIOR AUTHORIZATION ROI CALCULATOR
Calculate your savings
Enter in the number of prior authorization requests your team processes each month, the number of staff processing such requests, and the annual salary of each of your team members.
Check your inbox for results to see how much you can save by incorporating an AI-powered prior authorization solution at your organization.