
JOIN US AT NAHAM
Meet Us At Booth #511
At NAHAM Annual Conference 2023, you’ll reconnect with your colleagues while learning cutting-edge strategies for overcoming staffing challenges, inspiring team success, handling prior authorizations, and building a patient access career.
Exploring these critical concepts will light a fire under you, but keeping up that momentum after your return can be a challenge. A proven, knowledgeable partner helps you implement the profitable future you know you and your facility are capable of.
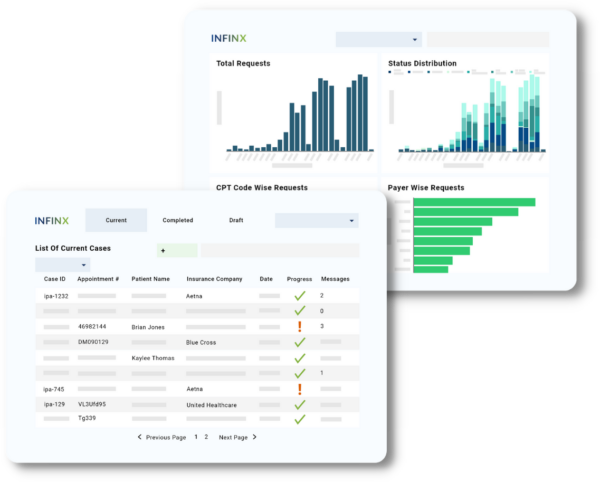
Our patient access and RCM solutions—powered by AI, automation, and trained specialists—enable patient access professionals to seamlessly intake, schedule, and care for patients. Given an industry-wide healthcare staffing shortage and tightening payer reimbursements, providers find augmenting staff capacity with technology and prior authorization experts helps them recoup the most revenue. This automation + specialists approach reinforces all patient access tasks, including document capture, eligibility and benefits verification, prior authorizations, and patient pay estimates.
Schedule a time to meet with us to gain insights on comprehensive or selective patient access solutions.
- Eligibility Verification
- Benefits Check
- Prior Authorization
- Insurance Discovery
- Patient Pay Estimation
- A/R Recovery
- Denials Management
- Charge Capture Optimization
- Revenue Insights
- Coding Support
NAHAM Symposium With Senior Patient Access Product Manager
Next-Generation Of AI-Based Solutions In Patient Access
With Senior Product Manager Aakarsh Sethi
May 4, 2023 | 11:30AM – 12:30 PM
Room Wekiwa 1-2
Rosen Shingle Creek Hotel
Providing timely and reliable patient care is the healthcare provider’s prime directive.
Unfortunately, inconsistencies in payer’s patient access processes and tightening restrictions often delay care, negatively impacting patient experience and making it harder for providers to get paid. In a recent AMA study, 33% of providers have shared that delaying care due to patient access bottlenecks had led to disability, hospitalization, and even death among their patient population. A smooth patient access process is critical to appropriate patient care.
Making sure that providers get paid for services rendered is also crucial. More providers are using technology and automation to support staff in ascertaining that a patient has an active payer policy, benefits, and accurate patient cost estimates. It even augments staff in obtaining prior authorizations— some of the most cost-intensive and manually laborious processes that a provider undertakes.
Citing the dire staffing shortage, healthcare leaders are urging providers to turn to technology to help ease the burden of patient access. Next-generation technologies, including those within artificial intelligence (AI), can help provide exponential value within the patient access space.
Join Aakarsh Sethi, Senior Product Manager at Infinx on May 4th, 11:30AM – 12:30PM for a symposium on how forward-thinking providers are leveraging AI-driven patient access technology to deliver prompt, thorough, appropriate care and get paid at appropriate levels for these services.
If you can’t attend Aakarsh’s talk, you can request a recording here. Indicate in a field that you’d like to receive the recording in your inbox. We’ll be happy to send it to you shortly after the conference.
Our Latest News
Escalate Patient Volume and Slash Denials With Patient Access Plus
Too many providers and groups are still treating patients before eligibility and benefits have been confirmed and prior authorizations approved. Patient access leaders and administrators are then left with prior authorization and claims denials that sap revenue.
Given a widespread staffing shortage, too often providers treat before establishing authorization, as [this case study](https://www.infinx.com/case-study/rural-midwest-hospital-improves-revenue-and-patient-satisfaction-with-end-to-end-patient-access-partnership/) explores. For those facilities that do seek prior authorization, delays can frustrate patients, prompting them to seek care elsewhere. Add these challenges to increasingly tight requirements from government entities and insurance companies, and providers face more obstacles to revenue capture than ever.
Only by leveraging artificial intelligence-powered technology plus patient access experts trained in specialty-specific revenue workflows can today’s providers speed and perfect insurance discovery, prior authorizations, patient pay estimates, and more tasks that get the schedule filled with financially-proven patients. As a patient access professional, you CAN help stem revenue leakage. Learn more from our team at booth #511 at the NAHAM 2023 Annual Conference.
- Prior Authorization
- Eligibility Verifications & Benefits Checks
- Patient Pay Estimates
- Insurance Discovery
- Patient Access Analytics
- Referral & Document Capture
- Prior Authorization Support For Referring Physicians
- Clinical Guidelines Search Tool
