The future of patient access in healthcare will be defined by technology and anchored in the rich triad of automation, artificial intelligence, and analytics…and it’s available today! At the recent National Association of Healthcare Access Management (NAHAM) Symposium, Natalia Arzeno, Chief Data Scientist, and Aakarsh Sethi, Product Manager, from Infinx Healthcare, presented a discussion on the impact of a reshaped and supercharged payment lifecycle and its impact on the business of healthcare.
During the presentation, the healthcare payment lifecycle pre and post-care processes were outlined in terms of preserving and maximizing revenue by leveraging technology to increase efficiencies. The discussion then focused in on the technological impact that data analytics, automation, and artificial intelligence is having on the patient access functions that lay the foundation during the pre-care phase for successful reimbursement at the highest levels.
Patient Access and the Healthcare Payment Lifecycle
Whether a patient is accessing healthcare through an ambulatory channel, such as a provider’s office, outpatient surgery center or urgent care center, or through inpatient care at a hospital, the healthcare payment lifecycle is relatively similar. The third-party payer system, long in effect in healthcare, creates a complex system for identifying, verifying, and codifying patient encounters and the exactness of the process has a direct impact on bottom-line revenue.
Specifically, understanding the pre-care patient access component from scheduling, through insurance authentication and prior authorization, to pre-collections, allows us to apply innovations in technology and machine learning to build better groundwork for a strong and effective post-care revenue cycle management process.
Technology Applications for Pre-Care Patient Access
Arzeno and Sethi first defined the three types of technology and outlined how each could benefit the process of patient access flow.
- Automation – eases the redundant human burdens and mimics the actions of the workforce. Automation is being used to determine insurance eligibility, prior authorization, and patient responsibility for pre-collections.
- Analytics – digital data collection designed to enhance productivity through analyzing patterns, trends, and statistical information. Data Analytics is being used to quantify outcomes based on performance and developing predictive scenarios to enhance healthcare payment lifecycle results.
- Artificial Intelligence (AI) – by identifying patterns through computational analyses, AI can make predictions that support and amplify those made by humans alone. For the pre-care patient access process, this means predicting risk and behavior, and forecasting potential outcomes.
Transforming Pre-Care Patient Access through Technology
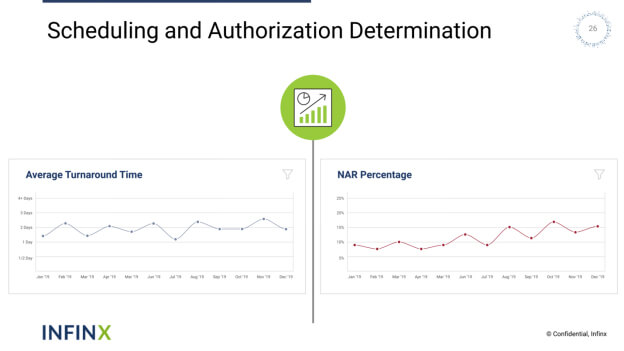
Scheduling and Authorization Determination – The process of patient scheduling is greatly enhanced when supported by technological advances. The scheduler can use an automated process to determine patient eligibility and insurance verification with the click of a button while making the appointment. Actionable prior authorization requirements can be returned immediately through AI, alleviating the scheduler from having to perform a manual search of what could be out-of-date insurance information.
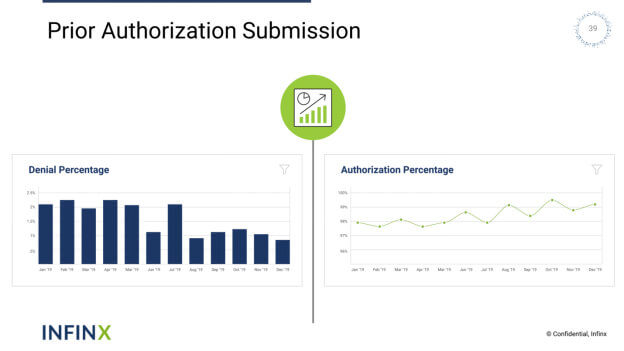
Prior Authorization Submission – Once prior authorization submission requirements have been determined, AI-enhanced software can then be utilized to determine risk and submit patient information to the insurance company. By automating prior authorization workflow, business office personnel can take the guesswork out of unnecessary re-handling of submissions.
Patient Payment – With upwards of 30% of payment responsibility now resting squarely with the patient, it’s more important than ever to have an early, well-defined plan for upfront payment. As part of the pre-collection process, the patient’s responsibility can be determined by the automated payment estimator component of the AI-driven prior authorization software. Then the AI software estimates what is due at the time of service and assesses the patient’s ability to pay. With this real-time information in hand, personnel can determine a course of action regarding payment disposition.
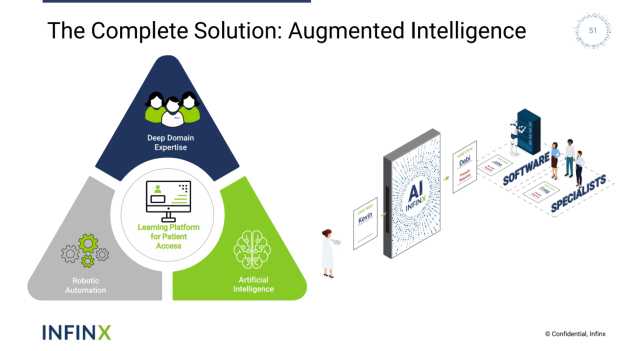
The Complete Solution: Augmented Intelligence
Through Infinx’s comprehensive prior authorization software utilizing robotic automation, artificial intelligence, and deep domain expertise, a healthcare organization’s payment life cycle can be given a solid infrastructure for processing and successfully collecting its revenue due in an ever-tightening marketplace. Whether absorbing manual processes through automation or enlisting software with machine learning capabilities, these solutions have a positive and quantifiable effect on bottom-line revenue.
Contact Infinx today to schedule a demo to explore how prior authorization software can work for you!