Key Takeaways:
-
Many performance indicators can be automatically tracked and routinely analyzed to tell the story of an organization’s financial health and wellbeing.
-
Keeping a KPI Scorecard allows you to keep a closer eye on routine follow up and collections, as well as monitoring root causes impacting reimbursement.
-
There are seven revenue cycle metrics that ensure your team is doing the best job possible and securing every dollar that’s owed.
There’s a famous quote from Peter Drucker, author and management consultant, that will always hold true in business – “If you can’t measure it, you can’t improve it.” His words are especially true when evaluating the healthcare payment lifecycle and Revenue Cycle Management (RCM) systems within any hospital or physician’s practice.
The healthcare industry has an increasingly complicated reimbursement system that is unlike any other sector in business. With federal and state regulations and oversight, third-party payers—each with their own set of rules and adjustments—and a codification system that is multi-layered, intricate and complex, hospitals and physicians are challenged at every turn.
7 Key Areas for RCM Metrics Found in Claim Analytics
With the level of sophisticated automation available today, many different categories of information and performance indicators can be automatically tracked and routinely analyzed to tell the story of an organization’s financial health and wellbeing.
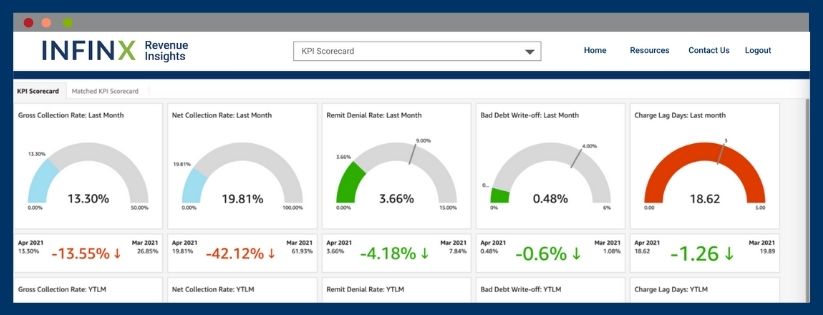
Keeping a KPI Scorecard, such as the one available through Infinx Healthcare, allows you to maximize your reimbursement by keeping a closer eye on routine follow up and collections, as well as discovering, correcting, and monitoring root causes impacting reimbursement.
In a recent Medical Group Management Association (MGMA) article, 69% of healthcare participants reported that their denials have increased by an average of 17% in 2021. The report went on to say that the cost of reworking denied claims was about $25 per claim and that over 50% of denied claims are simply written off with no attempt to correct or resubmit.
By leveraging AI and the strength of machine learning, revenue cycle teams are given timely, actionable insights that focus on the inventory of claims through healthcare analytics and claim analytics. The Infinx Revenue Insights Solution Guide (IRIS) gives a hospital or practice a complete dashboard-based look at their results and focuses their future efforts in resolving and collecting outstanding claims.
Of the many metrics available for quantification, these seven categories are preeminent and should be available in real-time at any time:
- Gross Collections Rate (GCR): A percentage of collections based on the total amount billed for all services and hard goods. In healthcare, this metric is important to evaluate the effectiveness of your collections efforts, but also to maintain the effectiveness of your overall contracting with insurance companies.
- Net Collections Rate (NCR): A percentage that compares your net collections to the amount contractually allowed by insurance. If the amount is too low (below 90-92%), then money is not being followed up on that should be collectible.
- Denial Rates: The denial rate represents, as a percentage, claims that are denied by insurance payers during a specific period of time. If this rate is over 5%, there is a good chance that denials have been received, but not followed up on in a timely manner.
- Write-Offs: The write-off percentage lets you know the effectiveness of your collections efforts. This percentage is the way to ensure that your insurance payer reimbursement is in line with contractual agreements and is also a way to monitor that denials are being appropriately followed up and collected.
- Charge Lag Days: This calculation looks at the number of days from the patient’s date of service to the date the claim is filed. Ideally, this should be the same or next day. If there is a delay, whether from providers not preparing their charges efficiently or staff not processing and filing claims effectively, this metric gives the best indication of pre-filing workflow.
- Days Outstanding in A/R: A measurement of how long claims are in A/R prior to final collections, and one that can be positively impacted by tightening pre-service collections to reduce the amount due by patients after all insurance has been resolved.
- Percentage of A/R over 90 Days: This percentage is a clear indicator of the effectiveness of your hospital or practice collections procedures. The lower this number the more efficient reimbursement is being handled. Additionally, any amounts due that are still outstanding after 90 days become less collectible each day.
Having solid auditing and compliance procedures for these seven revenue cycle metrics is a significant way to ensure that you are doing the best job possible and securing every dollar that’s owed to your organization. It’s also a great communication tool when working with providers or employees in setting expectations and creating accountability.
Monitoring performance is critical in today’s healthcare reimbursement arena and employing a full RCM Platform, like Infinx Healthcare offers, allows you to monitor numerous metrics and claim analytics (including these 7 indicators) as well as optimizing A/Rs through recovery prediction, smart prioritization, denial workflow, and shortfall detection powered by artificial intelligence, machine learning and robotic process automation.
Request a demo today to learn more about Infinx Healthcare’s RCM Platform and our Revenue Insights (IRIS) analytics module, and evaluate your RCM Metrics.